This Week in Dental Implants, we are presenting a case demonstrating the use of a new material, the DALI Flex Graft, to help simplify contour augmentation around an implant to address a ridge deficiency.
Background: Contour Augmentation is Essential
Contour augmentation around a ridge deficiency for an implant is essential not only for aesthetic reasons, but also for the functional success and longevity of dental implants.
In terms of esthetics, it helps to restore the natural anatomy of the alveolar ridge, which is essential for achieving optimal aesthetic outcomes. When there is a deficiency, the final crown may appear unnatural due to irregularities in the underlying bone structure, leading to poor soft tissue support and an unesthetic emergence profile.
Perhaps, more importantly, though, adequate contour augmentation can enhance the stability of the implant. By correcting underlying bony defects, the surrounding soft tissue can be better supported, which is vital for maintaining the integrity of the implant over time. Specifically, contour augmentation helps prevent vertical bone loss,1 and minimizes complications such as mucosal recession2. Additionally, implant thread exposure is a risk indicator for peri-implantitis, and so treating the defect can reduce the risk of peri-implantitis. 3
Various materials and methods have been suggested for contour augmentation to address defects, with the classic plan involving placement of particulate graft and a membrane (either resorbable or non-resorbable). However, these techniques, while yielding positive clinical results, are not necessarily easy and without potential complications. For example, when using a membrane the bone growth depends on the ability of the membrane to maintain its structural integrity.4,5,6,7,8,9
Because of some of the difficulties faced in employing the traditional methods, DALI developed a flexible cortical graft, the DALI Flex Graft.. It is a 1 mm thick demineralized cortical allograft that when hydrated, becomes flexible and easily adapts to graft sites that would be difficult to treat with particulate or putty grafts. These characteristics make DALI Flex Graft ideally suited for the repair of shallow bone defects around implants. The case below demonstrates the use of the DALI Flex Graft to successfully address residual lack of ridge contour.
Case Presentation
Case Presented By: Dr. Daniel Gober, Marine Park Perio
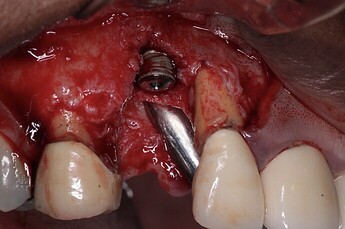
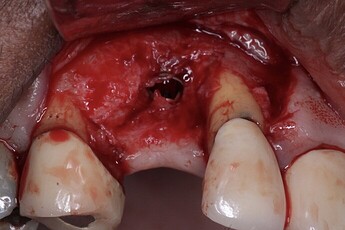
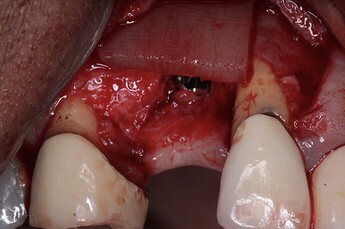
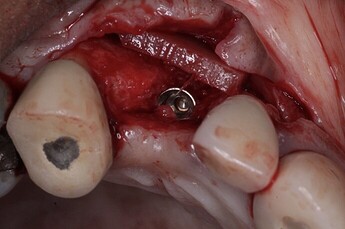
At the time of the original implant placement a classic GBR procedure was performed with DALI Mineralized Cortical/Cancellous and a collagen membrane. (Pictures 1,2,3). However, a buccal ridge deficiency persisted (Picture 4). Surgical uncovery of the implant to expose the cover screw did reveal successful bone regeneration around the implant, but a residual lack of ridge contour was noted (Picture 5).
Instead of using a traditional particulate graft covered with a resorbable membrane, a “flexible bone graft” sheet, the DALI Flex Graft, was placed over the buccal plate to augment the buccal contour (Pictures 6 & 7). Because the graft comes hydrated, it is easy to handle and adapt to the defect location. The flap was then pulled over the graft and adapted around the healing abutment (Picture 8).
After a six-week healing period, we observed see nice healing and an obvious increase in the facial contour (Picture 9). Subsequently, an impression was taken and the implant was restored with a screw-retained crown (Picture 10).
This case demonstrates that utilizing the DALI Flex Graft cortical bone sheet is a more manageable and effective way to address this type of defect, when compared to the conventional particulate graft + barrier membrane approach.
References
1. A randomized controlled clinical trial comparing small buccal dehiscence defects around dental implants treated with guided bone regeneration or left for spontaneous healing., Ronald E Jung , Milan Herzog , Karin Wolleb , Christian F Ramel , Daniel S Thoma , Christoph H F Hämmerle , Clinical oral implants research. Volume: 28, Issue: 3, 2017
PURPOSE
The aim of the present randomized controlled clinical study was to test whether small bony dehiscence defects (≤5 mm) left to heal spontaneously result in the same clinical and radiological outcome as defects treated with guided bone regeneration (GBR).
MATERIALS AND METHODS
Twenty-two patients who received at least one implant with a small bony dehiscence defect were enrolled in the study. If the defect height was ≤5 mm, the site was randomly assigned to either the spontaneous healing (SH) group or the GBR group. In the SH group, the defect was left without any treatment. In the GBR group, the defects around the implants were grafted with deproteinized bovine bone mineral (DBBM) and covered with a native collagen membrane. Clinical and radiographic measurements were performed 6 months after implant placement with a reentry surgery and at the time of crown insertion and the subsequent follow-up appointments at 3, 6, 12 and 18 months after loading. For statistical analyses, the mixed linear model was applied for the clinical and radiographic measurements observed around the implants. Simple comparisons of the location of the measurements in the two independent groups are performed with the Mann-Whitney U-test. In addition, the mixed model assumptions were checked.
RESULTS
The implant and crown survival rate 18 months after loading was 100%, revealing no serious biologic or prosthetic complication. The mean changes of the buccal vertical bone height between implant placement and reentry surgery after 6 months revealed a small bone loss of -0.17 ± 1.79 mm (minimum -4 mm and maximum 2.5 mm) for the SH group and a bone gain of 1.79 ± 2.24 mm (minimum of -2.5 mm and maximum of 5 mm) for the GBR group, respectively (P = 0.017). Radiographic measurements demonstrated a slight bone loss of -0.39 ± 0.49 mm for the SH group and a stable bone level of 0.02 ± 0.48 mm for GBR group after 18 months. All peri-implant soft tissue parameters revealed healthy tissues with no difference between the two groups.
CONCLUSION
Small bony dehiscence defects left for spontaneous healing demonstrated high implant survival rates with healthy and stable soft tissues. However, they revealed more vertical bone loss at the buccal aspect 6 months after implant insertion and also more marginal bone loss between crown insertion and 18 months after loading compared to sites treated with GBR. Read More
2. Influence of buccal bone wall thickness on the peri-implant hard and soft tissue dimensional changes: A systematic review., Alberto Monje , Andrea Roccuzzo , Daniel Buser , Hom-Lay Wang , Clinical oral implants research. Volume: 34, Issue: 3, 2023
BACKGROUND
The significance on the association between the peri-implant bucco-lingual dimension (BLD) at the stage of implant placement and the occurrence of biological and esthetic complications is yet unknown.
MATERIAL AND METHODSS
Systematic screening of electronic sources was carried out to identify clinical and preclinical studies reporting on the baseline BLD and/or buccal bone thickness (BBT) values. A secondary objective was to assess the effect of simultaneous grafting at sites with deficient or no buccal bone wall (BBW) at baseline. The primary outcome variables were BBT, BLD, and buccal vertical bone loss (VBL) at re-evaluation. Moreover, radiographic, clinical, and patient-reported outcome measures (PROMs) were evaluated.
RESULTS
Overall, 12 clinical and four preclinical studies met the inclusion criteria. Inconsistencies were found in defining the critical BBT across the clinical and preclinical data evaluated. The clinical evidence demonstrated that during healing, dimensional changes occur in the alveolar bone and in the BBW that may compromise the integrity of the peri-implant bone, leading to VBL and mucosal recession (MR), particularly in scenarios exhibiting a thin BBW. The preclinical evidence validated the fact that implants placed in the presence of a thin BBW, are more prone to exhibit major dimensional changes and VBL. Moreover, the clinical data supported that, in scenarios where dehiscence-type defects occur and are left for spontaneous healing, greater VBL and MR together with the occurrence of biologic complications are expected. Furthermore, the augmentation of dehiscence-type defects is associated with hard and soft tissue stability. PROMs were not reported.
CONCLUSIONS
Dimensional changes occur as result of implant placement in healed ridges that may lead to instability of the peri-implant hard and soft tissues. Sites presenting a thin BBW are more prone to exhibit major changes that may compromise the integrity of the buccal bone and may lead to biologic and esthetic complications. Read More
3. Interproximal implant thread exposure after initial bone remodeling as a risk indicator for peri-implantitis., Andrea Ravidà , Ankita Samal , Musa Qazi , Liana Preto Webber , Hom-Lay Wang , Pablo Galindo-Moreno , Wenche S Borgnakke , Muhammad H A Saleh , Journal of periodontology. Volume: 94, Issue: 6, 2023
BACKGROUND
Due to the clinical challenges involved in successfully treating peri-implantitis, it is imperative to identify patient- and implant-level risk factors for its prevention. The main goal of this retrospective longitudinal radiographic and clinical study was to investigate whether interproximal radiographic implant thread exposure after physiological bone remodeling may be a risk factor for peri-implantitis. The secondary goal was to evaluate several other potential risk indicators.
METHODS
Of 4325 active dental school patients having implants placed, 165 partially edentulous adults (77 men, 88 women) aged 30-91 with ≥2 years of follow-up upon implant restoration were included. Implants with ≥1 interproximal thread exposed (no bone-to-implant contact) (n = 98, 35%) constituted the test group and those without exposed threads (n = 182, 65%) the control group. Descriptive, binary, and multivariate regression analyses were evaluated for goodness of fit. Wald tests were used to evaluate for significance set at 0.05.
RESULTS
Of the 280 implants (98 test, 182 control), 8 (2.9%) failed over a mean follow-up period of 7.67 (±2.63) years, and 27 implants (19 test, 8 control) developed peri-implantitis, with the exposed group having eight-fold (7.82 times) adjusted greater odds than the non-exposed. The risk increased four-fold (3.77 times) with each thread exposed. No other patient- or implant-related potentially confounding risk factors were identified.
CONCLUSIONS
Exposed interproximal implant threads after physiologic bone remodeling may be an independent risk indicator for incident peri-implantitis. Hence, clinicians should closely monitor patients with implant threads that have no bone-to-implant contact for incident peri-implantitis. Read More
4. Esthetic grafting for small volume hard and soft tissue contour defects for implant site development., Bach Le , Jeffrey Burstein , Implant dentistry. Volume: 17, Issue: 2, 2008
Ridge contour defects around dental implants are caused by underlying bony defects. Although adequate bone may exist to obtain stability of the implant, irregular bony anatomy can result in an unnatural appearance of the final crown. Particulate onlay grafting to support the peri-implant soft tissue along with tension-free closure while using pedicle papilla regeneration techniques can convert unaesthetic gingival contours into favorable sites. Read More5. The Aesthetic Contour Graft - Enhancing peri-implant soft tissue contours and pontic sites with guided bone regeneration., Bach Le , Naoki Hayashi , Journal of esthetic and restorative dentistry : official publication of the American Academy of Esthetic Dentistry ... [et al.]. Volume: 34, Issue: 1, 2022
OBJECTIVE
In this article, we will discuss strategies for enhancing peri-implant soft tissue contours and pontic sites with hard tissue augmentation.
CLINICAL CONSIDERATION
One of the keys to the esthetic illusion of an implant-supported restoration is to create an ideal emergence profile. A critical part of any emergence profile is based on the height and thickness of the tissue surrounding the restoration and whether there are any defects in this tissue. Even when there is adequate bone in which to place implants, if any irregular ridge anatomy that supports this tissue is not corrected, then an unesthetic appearance of the restoration can result due to the lack of soft tissue with which to develop a proper emergence profile.
CONCLUSION
Most peri-implant soft tissue deficiencies represent an underlying bony defect that can be corrected or enhanced through bone augmentation.
CLINICAL SIGNIFICANCE
Traditional methods of enhancing soft tissue emergence profiles around implants and pontic sites mostly involve the use of soft tissue augmentation techniques. Although there are few reports of the use of bone augmentation for this purpose, soft tissue contours can be enhanced by augmenting the underlying bone contours and, in many instances, may obviate the need for subsequent soft tissue augmentation. Read More
6. Effectiveness of Contour Augmentation with Guided Bone Regeneration: 10-Year Results., V Chappuis , L Rahman , R Buser , S F M Janner , U C Belser , D Buser , Journal of dental research. Volume: 97, Issue: 3, 2018
In aesthetic sites, the integrity of the facial bone wall dimension in the anterior maxilla is jeopardized by physiologic and structural changes postextraction. An effective regenerative protocol is key to reestablish and maintain the hard and soft tissue dimensions over time. The present prospective case series study examined the effectiveness of early implant placement with simultaneous contour augmentation through guided bone regeneration with a 2-layer composite graft in postextraction single-tooth sites over an observation period of 10 y among 20 patients. The median peri-implant bone loss was 0.35 mm between the 1- and 10-y examination. A success rate of 95% was obtained, with pleasing aesthetic outcomes and a high median Pink Esthetic Score (8). Implant crowns (ICs) revealed significant median facial recession between IC and IC (0.17 mm). The facial bone wall dimensions were assessed by preoperative cone beam computed tomography and 2 subsequent scans taken at 6 and 10 y. The median facial bone wall thickness increased significantly from 0 mm at surgery to 1.67 mm at the 10-y examination. The facial vertical bone wall peak (DIC) was located at a median distance of 0.16 mm coronal to the implant shoulder. The facial vertical bone loss of DIC amounted to 0.02 mm between 6 and 10 y. Equivalence testing was performed for the null hypothesis of a difference of >0.2 mm per year between 2 respective time points, showing stable bone conditions. Modulating factors influencing the regenerative outcomes at 10 y were the preoperative proximal crest width and soft tissue thickness. In conclusion, the present study confirmed the long-term effectiveness of early implant placement with simultaneous contour augmentation through guided bone regeneration with a 2-layer composite graft in postextraction single-tooth sites offering stable bone conditions with low risks of mucosal recessions over an observation period of 10 y ( ClinicalTrials.gov NCT03252106). Read More7. Augmentation procedures for the rehabilitation of deficient edentulous ridges with oral implants., Matteo Chiapasco , Marco Zaniboni , Maurizio Boisco , Clinical oral implants research. Volume: 17 Suppl 2, Issue: , 2006
OBJECTIVES
To analyze publications related to augmentation procedures and to evaluate the success of different surgical techniques for ridge reconstruction and the survival/success rates of implants placed in the augmented areas.
MATERIAL AND METHODS
Clinical investigations published in English involving at least 5 patients and with a minimum follow-up of 6 months were included. The following procedures were considered: a) Guided bone regeneration (GBR); 2) Onlay bone grafts; 3) Inlay grafts; 4) Bone splitting for ridge expansion (RE); 5) Distraction osteogenesis (DO); and 6) Revascularized flaps. Success rates of augmentation procedures and related morbidity, as well as survival and success rates of implants placed in the augmented sites were analyzed.
RESULTS
Success rates of surgical procedures ranged from 60% to 100% for GBR, from 92% to 100% for onlay bone grafts, from 98% to 100% for ridge expansion techniques, from 96,7% to 100% for DO, and was 87.5% for revascularized flaps, whereas survival rates of implants ranged from 92% to 100% for GBR, from 60% to 100% for onlay bone grafts, from 91% to 97.3% for RE, from 90.4% to 100% for DO, and, finally, was 88.2% for revascularized flaps.
CONCLUSION
On the basis of available data it was shown that it was difficult to demonstrate that a particular surgical procedure offered better outcome as compared to another. The main limit encountered in this review has been the overall poor methodological quality of the published articles. Therefore larger well-designed long term trials are needed. Read More