This Week in Dental Implants, we are highlighting a really interesting study from Urban et al. that investigated the use of newer perforated titanium‐reinforced dense‐polytetrafluoroethylene (PTFE) mesh when covered with a collagen membrane. 1 The aim of the study was to evaluate the non‐inferiority of perforated Titanium‐reinforced PTFE Membranes alone compared with Titanium‐reinforced PTFE Membranes covered with collagen membranes in vertical ridge augmentation procedures. Case photos with both techniques are shown below.
With a plethora of options for membranes, it is always elucidating to read up on newer techniques and thereby reinforce the general principles which guide every day clinical decisions.
Background on Titanium‐reinforced PTFE Membranes
The use of a membrane in guided bone regeneration is considered an essential tool for successful guided bone regeneration (GBR)/guided tissue regeneration (GTR). There are various different types of membranes, both resorbable and non-resorbable, that have been used clinically and many studies have been done highlighting the positives and negatives for all of the different materials.
One particularly important innovation in GBR was the introduction of Titanium‐reinforced PTFE Membranes. These membranes offer all the classic benefits of PTFE membranes, but the titanium reinforcement provides additional structural support, which helps maintain the space needed for bone regeneration. This is crucial in preventing the collapse of the membrane (notably collagen membranes are prone to deformation) and ensuring adequate bone growth. The rigidity provided by the titanium reinforcement also aids in maintaining the desired shape and position of the membrane, which is important for the stability of the underlying graft material and the overall success of the procedure.
In an extensive overview of all the different membranes used for vertical bone regeneration, Zhang M et al. 2 concluded that:
Based on this series of comprehensive analyses, it was determined that the application of a titanium-reinforced e-PTFE membrane in GBR/GTR may be the best choice.
Of course, there are downsides to non-resorbable membranes (e.g. they require a second surgery for removal) and they are not indicated or desired in every situation, so blindly accepting the conclusion above is not advised. Nevertheless, we highly recommend reading the study, Effect of Different Membranes on Vertical Bone Regeneration: A Systematic Review and Network Meta-Analysis as it provides an amazing overview of all the different types of membranes, and ranks them on effectiveness.
The Advent of Perforated Titanium‐reinforced PTFE Membranes: Improving Vascularization but with a Catch
Despite the demonstrated effectiveness of Titanium‐reinforced PTFE Membranes in vertical ridge augmentation, one concern with these membranes it that they may hinder vascularization from the periosteal vessels of the flap covering the defect. The periosteum contains a rich network of blood vessels that supply essential nutrients and oxygen to the surrounding tissues, which are vital for the healing process after surgical interventions. Adequate vascularization can reduce the risk of complications, which can arise from insufficient blood supply. Studies have shown that the use of periosteal vascular flaps significantly increases bone augmentation in both vertical and horizontal dimensions, highlighting the importance of vascularization in achieving successful outcomes in ridge augmentation procedures.
This issue with vascularization has led to the development of newer perforated Ti‐reinforced membranes. The open pores in these membranes enhance the revascularization of the bone graft from the surgical flap, and in that appear to offer “the best of both worlds.” There aren’t many studies on these newer perforated membranes, but one study 3 summarized the research as follows:
The increased permeability of membranes in the perforated group potentially enabled periosteal precursor cells to have greater access to rhBMP-2. The availability may have accelerated their differentiation into mature bone-forming cells, contributing to the stimulation of new bone production relative to the nonperforated group.
While perforation of the Ti‐reinforced membranes appears to improve revascularization, this benefit seems to be outweighed by the fact that the pores at the same time reduce the membrane’s ability to act as a complete cell barrier, which is essential for successful GBR.
Adding a Collagen Membrane to the Mix?
To compensate for this possible downside of the reduced barrier properties of the perforated membranes, it is generally recommended to use a collagen membrane along with the Perforated Titanium‐reinforced PTFE Membranes to improve the barrier function.
This brings us to the current study, which is the first of its kind to investigate whether you should cover these newer perforated membranes or not. The hypothesis was that PTFE alone (test group) would not be inferior to PTFE + Collagen Membrane (control group) in terms of absolute vertical bone gain.
Our Take: Study Results Support the Dual Membrane Technique of PTFE + Collagen, making the Cost/Benefit Analysis of Perforated Membranes Tricky
Reading, the results of non-inferior based studies is always confusing, because of the substantial use of double negatives. This study was no exception, with the conclusion stating that: “Non‐inferiority was not shown”, which applying the double negative, translates into the conclusion that using the perforated membranes alone without a collagen membrane is possibly inferior. The actual conclusion:
The non‐inferiority of PTFE mesh alone compared with PTFE mesh covered with a collagen membrane, in terms of absolute VBG, was not established. However, superiority analysis demonstrated that both techniques yielded comparable outcomes in terms of VBG, complication rates and bone density. Furthermore, the higher incidence of type 1 pseudo‐periosteum and LBV in the PTFE + CM group suggests that the addition of a collagen membrane may help prevent soft tissue ingrowth.
As always, reading the conclusion alone can be somewhat misleading, so please be sure to check out the whole study at: Impact of Collagen Membrane in Vertical Ridge Augmentation Using Ti-Reinforced PTFE Mesh: A Randomised Controlled Trial. Nevertheless our takeaway from this study is simply that if you are going to use these new perforated membranes, you are best advised to do so in combination with a collagen membrane.
We will keep an eye out for newer studies on these newer perforated membranes, but from our perspective, the need to use these in combination with a collagen membrane will greatly increase the overall treatment cost for what is still an unproven benefit of perforation. As such, given the unknown cost/benefit, we think the adoption rate of these newer perforated membranes will be slow, and clinicians are advised for now to stick to their current armamentarium, which may include the non-perforated Titanium‐reinforced PTFE Membranes, due to their superior results in many studies.
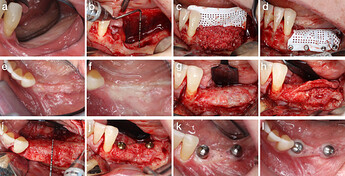
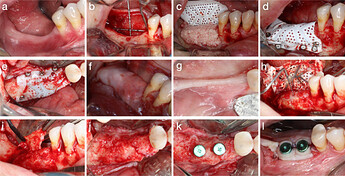
Case Presentation
Cases Images below are from from Urban IA, Serroni M, Dias DR, Baráth Z, Forster A, Araújo TG, Saleh MHA, Cucchi A, Ravidà A. Impact of Collagen Membrane in Vertical Ridge Augmentation Using Ti-Reinforced PTFE Mesh: A Randomised Controlled Trial. J Clin Periodontol. 2025 Apr;52(4):575-588. doi: 10.1111/jcpe.14129. Epub 2025 Feb 14. PMID: 39953742; PMCID: PMC11949596.
Representative case from the PTFE group with a step‐by‐step demonstration of the surgical procedure. (a) Pre‐operative buccal view of a posterior mandibular area that required vertical GBR. (b) Measurements of the vertical dimensions of the defect. (c) A titanium‐reinforced PTFE membrane was fixed in place after decortication of the recipient site and placement of particulate deproteinized bovine bone mineral combined with autogenous graft (1:1 ratio). (d) Buccal view of the titanium‐reinforced PTFE membrane fixed in place with titanium pins and screws. Coronal flap advancement was obtained before closure. Tension‐free flap closure was performed using the double‐layer suturing technique. (e, f) Clinical view of the regenerated area 9 months after surgery. (g) Re‐entry surgery after flap and membrane elevation; intra‐operative evaluation of pseudo‐periosteum formation and bone density. (h) Pseudo‐periosteum removal. (i) Occlusal view of the defect after GBR, noting the excellent dimensions and vital‐looking ridge. (j) Two implants in place in biologically and prosthetically ideal positions. (k, l) Buccal and occlusal views after 3 weeks, demonstrating adequate implant position following successful VBA.
Representative case from the PTFE + CM group with a step‐by‐step demonstration of the surgical procedure. (a) Pre‐operative buccal view of a posterior mandibular area requiring vertical GBR. (b) Measurements of the vertical dimensions of the defect. (c) A titanium‐reinforced PTFE membrane was fixed in place after decortication of the recipient site and placement of particulate deproteinized bovine bone mineral combined with autogenous graft (1:1 ratio). (d, e) Buccal and occlusal views of the titanium‐reinforced PTFE membrane fixed in place with titanium pins and screws. (f) Native collagen membrane covering the defect without stabilisation. Coronal flap advancement was obtained before closure. Tension‐free flap closure was performed using the double‐layer suturing technique. (g) Clinical view of the regenerated area 9 months after surgery. (h) Re‐entry surgery after flap and membrane elevation; intra‐operative evaluation of pseudo‐periosteum formation and bone density. (i) Pseudo‐periosteum removal. (j) Occlusal view of the defect after GBR, showing the excellent dimensions and vital‐looking ridge. (k) Two implants in place in biologically and prosthetically ideal positions. (l) Buccal view after suture, demonstrating adequate implant position following successful VBA.
References
1. Impact of Collagen Membrane in Vertical Ridge Augmentation Using Ti-Reinforced PTFE Mesh: A Randomised Controlled Trial., Istvan A Urban , Matteo Serroni , Debora R Dias , Zoltán Baráth , Andras Forster , Tiago G Araújo , Muhammad H A Saleh , Alessandro Cucchi , Andrea Ravidà , Journal of clinical periodontology. Volume: 52, Issue: 4, 2025
AIMS
This non-inferiority randomised clinical trial aimed to compare vertical bone gain (VBG), volumetric bone changes and incidence of complications after vertical ridge augmentation (VRA) using perforated titanium-reinforced dense-polytetrafluoroethylene (PTFE) mesh covered by a collagen membrane (CM) or used alone.
MATERIALS AND METHODS
Thirty patients with vertical bone defects were randomly assigned to receive VRA with either PTFE + CM or PTFE alone. Meshes were removed after 9 months. Clinical assessments included complication rates, pseudo-periosteum type and bone density. VBG, effective regeneration rate and the need for additional augmentation were evaluated using CBCT reconstructions.
RESULTS
Non-inferiority of PTFE alone compared with PTFE + CM was not demonstrated for absolute and relative VBG (4.5 ± 2.1 mm vs. 4.1 ± 2.7 mm, 79.2% ± 16.6% vs. 85.8% ± 10.6%, respectively), effective regeneration rates (69.3% ± 17.9% vs. 72.3% ± 16.4%, respectively) or complication rates (6.7% in both groups). A higher incidence of type 1 pseudo-periosteum was observed in the PTFE + CM group.
CONCLUSION
The non-inferiority of PTFE alone compared with PTFE + CM for absolute VBG was not established. However, both techniques led to comparable outcomes for VBG, complication rates and bone density. The higher incidence of type 1 pseudo-periosteum and lacking bone volume in the PTFE + CM group suggests that adding a collagen membrane may help prevent soft tissue ingrowth.
TRIAL REGISTRATION
Clinicaltrials.gov identification number: NCT04843488. Read More
2. Effect of Different Membranes on Vertical Bone Regeneration: A Systematic Review and Network Meta-Analysis., Mi Zhang , Zili Zhou , Jiahao Yun , Rui Liu , Jie Li , Yimeng Chen , HongXin Cai , Heng Bo Jiang , Eui-Seok Lee , Jianmin Han , Yunhan Sun , BioMed research international. Volume: 2022, Issue: , 2022
This study is aimed at performing a systematic review and a network meta-analysis of the effects of several membranes on vertical bone regeneration and clinical complications in guided bone regeneration (GBR) or guided tissue regeneration (GTR). We compared the effects of the following membranes: high-density polytetrafluoroethylene (d-PTFE), expanded polytetrafluoroethylene (e-PTFE), crosslinked collagen membrane (CCM), noncrosslinked collagen membrane (CM), titanium mesh (TM), titanium mesh plus noncrosslinked (TM + CM), titanium mesh plus crosslinked (TM + CCM), titanium-reinforced d-PTFE, titanium-reinforced e-PTFE, polylactic acid (PLA), polyethylene glycol (PEG), and polylactic acid 910 (PLA910). Using the PICOS principles to help determine inclusion criteria, articles are collected using PubMed, Web of Science, and other databases. Assess the risk of deviation and the quality of evidence using the Cochrane Evaluation Manual, and GRADE. 27 articles were finally included. 19 articles were included in a network meta-analysis with vertical bone increment as an outcome measure. The network meta-analysis includes network diagrams, paired-comparison forest diagrams, funnel diagrams, surface under the cumulative ranking curve (SUCRA) diagrams, and sensitivity analysis diagrams. SUCRA indicated that titanium-reinforced d-PTFE exhibited the highest vertical bone increment effect. Meanwhile, we analyzed the complications of 19 studies and found that soft tissue injury and membrane exposure were the most common complications. Read More3. Elucidating the Benefit of Perforated vs Nonperforated Membranes in Guided Bone Regeneration: An In Vivo Histologic Evaluation and Histomorphometric Analysis., Istvan A Urban , Nicholas Mirsky , Matteo Serroni , Nick Tovar , Vasudev Vivekanand Nayak , Lukasz Witek , Charles Marin , Muhammad H A Saleh , Andrea Ravidà , Istvan Baczko , Laszlo Parkanyi , Katalin Nagy , Paulo G Coelho , The International journal of periodontics & restorative dentistry. Volume: 45, Issue: 3, 2025
Nonperforated polytetrafluoroethylene (PTFE) membranes are effectively utilized in guided bone regeneration (GBR) but may hinder cell migration due to limited interaction with the periosteum. This study compared bone regeneration using occlusive or perforated membranes combined with acellular collagen sponge (ACS) and recombinant human bone morphogenetic protein-2 (rhBMP-2) in a canine mandibular model. Male Beagle dogs (n = 3) received two mandibular defects each to compare ACS/rhBMP-2 with experimental (perforated group) and control (nonperforated group) membranes (n = 3 defects/group). Tissue healing was assessed histomorphologically, histomorphometrically, and through volumetric reconstruction using microcomputed tomography. The perforated group showed increased bone formation and reduced soft tissue formation compared to the nonperforated group. For the primary outcome, histomorphometric analysis revealed significantly greater total regenerated bone in the perforated group (67.08% ± 6.86%) than the nonperforated group (25.18% ± 22.44%) (P = .036). Perforated membranes had less soft tissue infiltration (32.91% ± 6.86%) than nonperforated membranes (74.82% ± 22.44%) (P = .036). The increased permeability of membranes in the perforated group potentially enabled periosteal precursor cells to have greater access to rhBMP-2. The availability may have accelerated their differentiation into mature bone-forming cells, contributing to the stimulation of new bone production relative to the nonperforated group. Read More4. The use of e-PTFE barrier membranes for bone promotion around titanium implants placed into extraction sockets: a prospective multicenter study., W Becker , C Dahlin , B E Becker , U Lekholm , D van Steenberghe , K Higuchi , C Kultje , The International journal of oral & maxillofacial implants. Volume: 9, Issue: 1, 1994 Jan-Feb
This multicenter study was conducted to determine the predictability for implants placed into immediate extraction sockets and augmented with e-PTFE barrier membranes. Forty-nine implants were placed in immediate extraction sockets. Initial and final defect measurements and the number of threads exposed were compared. Patients were followed up to 1 year after implant loading. Three implants were lost at the abutment connection surgery. The 1-year survival rate was 93.9%. Twenty barrier membranes became exposed and were removed prior to stage 2 surgery, while the remaining barriers were removed at abutment connection. The average defect bone formation for membrane-retained sites was 4.8 mm, while the average bone formation for sites in which the membranes were prematurely removed was 4.0 mm (P < .0001). At stage 2 surgery there was an average of 0.6 threads exposed (P < .001) for the membrane-retained sites and 2.6 threads for the early removal sites (NS). Forty-five pairs of nonstandardized radiographs were evaluated for bone loss after implant loading (average 7.5 months). The mesiodistal bone loss averaged 0.72 mm. Within the limits of this study, e-PTFE membranes will promote clinically and statistically significant amounts of bone around immediately placed implants. Retention of e-PTFE barriers until stage 2 surgery improves the amount of bone promoted around the implants. Read More5. Reconstruction of vertical alveolar ridge deficiencies utilizing a high-density polytetrafluoroethylene membrane /clinical impact of flap dehiscence on treatment outcomes: case series/., Daniel Palkovics , Fanni Bolya-Orosz , Csaba Pinter , Balint Molnar , Peter Windisch , BMC oral health. Volume: 22, Issue: 1, 2022
OBJECTIVES
The aim of this study was to evaluate the effects of membrane exposure during vertical ridge augmentation (VRA) utilizing guided bone regeneration with a dense polytetrafluoroethylene (d-PTFE) membrane and a tent-pole space maintaining approach by registering radiographic volumetric, linear and morphological changes.
METHODS
In 8 cases alveolar ridge defects were accessed utilizing a split-thickness flap design. Following flap elevation VRA was performed with tent-pole space maintaining approach utilizing the combination of a non-reinforced d-PTFE membrane and a composite graft (1:1 ratio of autogenous bone chips and bovine derived xenografts). Three-dimensional radiographic evaluation of hard tissue changes was carried out with the sequence of cone-beam computed tomography (CBCT) image segmentation, spatial registration and 3D subtraction analysis.
RESULTS
Class I or class II membrane exposure was observed in four cases. Average hard tissue gain was found to be 0.70 cm, ± 0.31 cm, and 0.82 cm, ± 0.40 cm, with and without membrane exposure resulting in a 17% difference. Vertical hard tissue gain averaged 4.06 mm ± 0.56 mm and 3.55 mm ± 0.43 mm in case of submerged and open healing, respectively. Difference in this regard was 14% between the two groups. Horizontal ridge width at 9-month follow-up was 5.89 mm ± 0.51 mm and 5.61 mm ± 1.21 mm with and without a membrane exposure respectively, resulting in a 5% difference.
CONCLUSIONS
With the help of the currently reported 3D radiographic evaluation method, it can be concluded that exposure of the new-generation d-PTFE membrane had less negative impact on clinical results compared to literature data reporting on expanded polytetrafluoroethylene membranes. Read More
6. A randomised controlled trial comparing the effectiveness of guided bone regeneration with polytetrafluoroethylene titanium-reinforced membranes, CAD/CAM semi-occlusive titanium meshes and CAD/CAM occlusive titanium foils in partially atrophic arches., Pietro Felice , Roberto Pistilli , Gerardo Pellegrino , Lorenzo Bonifazi , Subhi Tayeb , Massimo Simion , Carlo Barausse , International journal of oral implantology (Berlin, Germany). Volume: 17, Issue: 3, 2024
PURPOSE
To compare the clinical effectiveness of three different devices used in guided bone regeneration procedures for partially atrophic arches.
MATERIALS AND METHODS
A randomised controlled trial with three parallel arms was conducted. The study evaluated titanium-reinforced polytetrafluoroethylene membrane (PTFE group), semi-occlusive CAD/CAM titanium mesh (mesh group) and occlusive CAD/CAM titanium foil (foil group) in terms of surgical outcomes and complications as well as surgical times and surgeon satisfaction in 27 guided bone regeneration procedures, presenting results from 1 year post-implant placement.
RESULTS
Complications occurred in seven patients. No significant difference was found between the groups in terms of the occurrence of complications (P = 0.51), device exposure (P = 0.12) and implant failure (P = 0.650). Surgeon satisfaction varied significantly, with the PTFE group differing from the mesh (P = 0.003) and foil groups (P 0.001), but not between meshes and foils (P = 0.172). Surgical times also differed significantly, with longer times for PTFE membranes compared to meshes (P 0.001) and foils (P = 0.006), but with no difference between meshes and foils (P = 0.308). The mean reconstructed bone volume was 1269.55 ± 561.08 mm3, with no significant difference observed between the three groups (P = 0.815). There was also no significant difference for mean maximum height (6.72 mm, P = 0.867) and width (7.69 mm, P = 0.998). The mean marginal bone loss at 1 year after implant placement was 0.59 ± 0.27 mm.
CONCLUSIONS
Although this study provides valuable insights into the potential benefits of using different types of CAD/CAM devices, further research with larger sample sizes and longer follow-up periods is warranted to validate these findings.
CONFLICT-OF-INTEREST STATEMENT
The authors declare there are no conflicts of interest relating to this study. Read More
7. Vertical ridge augmentation with Ti-reinforced dense polytetrafluoroethylene (d-PTFE) membranes or Ti-meshes and collagen membranes: 3-year results of a randomized clinical trial., Alessandro Cucchi , Sofia Bettini , Paolo Ghensi , Antonino Fiorino , Giuseppe Corinaldesi , Clinical implant dentistry and related research. Volume: 25, Issue: 2, 2023
BACKGROUND
The present study aimed to evaluate hard and soft tissue parameters around implants placed in augmented posterior mandible, comparing Ti-reinforced d-PTFE membranes with Ti-meshes covered with collagen membranes, after 3 years of follow-up.
MATERIALS AND METHODS
Forty eligible patients were randomly assigned to group A (Ti-reinforced d-PTFE membrane) or group B (mesh covered with collagen membrane) for vertical ridge augmentation (VRA) and simultaneous implants. Implants were evaluated using specific peri-implant parameters for bone and soft tissues: probing pocket depth (PPD), modified plaque index (mPI), bleeding on probing (BoP), modified gingival index (mGI), thickness of keratinized tissue (tKT), width of keratinized tissue (wKT), fornix depth (FD), peri-implant bone level (PBL), interproximal bone peaks (IBP), marginal bone loss (MBL), interproximal bone loss (IBL).
RESULTS
A total of 28 patients with 79 implants were evaluated after 3 years of follow-up. The mean value of MBL was 0.70 mm (group A = 0.73 mm; group B = 0.71 mm), while mean IBL was 0.54 mm (group A = 0.64 mm; group B = 0.40 mm). The treatment with meshes resulted not inferior to PTFE and their clinical results appeared similar. A strong correlation between PBL and IBP was confirmed. Both study groups showed an increase of tKT and wKT values.
CONCLUSION
In the posterior mandible, VRA using both techniques provides stable PBLs up to 3 years. A correct soft tissue management and a strict professional oral hygiene protocol play a crucial role on peri-implant health over time. Read More