This Week in Dental Implants, we wanted to focus on the topic of placement of implants in infected sites, following the release of a new 2-to-12 year clinical study that compared the survival rate and the success rate of single tooth implants placed and restored immediately after extraction in non-infected, and infected sites.
Background
In general, immediate placement of implants in a fresh post-extraction socket is becoming a popular treatment option. However, in the case, of an active infection in the extraction site, the placement of an immediate implant is clinically debatable. Evidence, however, does suggest that implants can indeed be placed into sites with periapical and periodontal infections, provided certain protocols are followed. The most recent study that caught our attention, Single Tooth Immediate Extraction Placement and Provisionalization in the Esthetic Area: Infected vs. Non-Infected Sites. A 2-To-12 Year Retrospective Clinical Study 1, followed a specific protocol:
Flapless extraction, thorough debridement of the alveolus, immediate placement of the implant, particulate graft material insertion around the implant, resorbable membrane insertion in the facial aspect of the implant for all those cases in which the buccal plate was compromised, and immediate insertion of a screw-retained provisional FDP out of occlusion.
The study showed:
comparable implant survival rate between single tooth implants placed and restored immediately in a non-infected, acutely infected or chronically infected site.
Cases
Cases by: Çolak S, Demïrsoy MS. Retrospective analysis of dental implants immediately placed in extraction sockets with periapical pathology: immediate implant placement in infected areas.
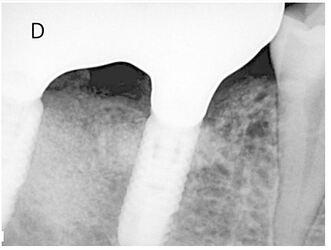
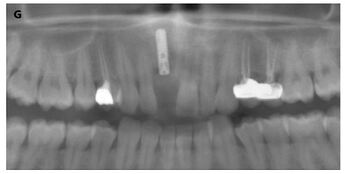
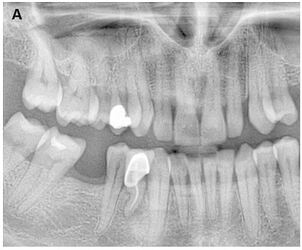
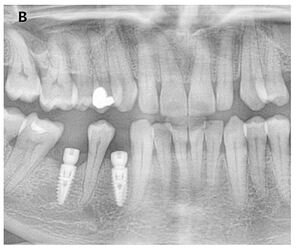
(A ) Right mandibular first and second molars with chronic periapical pathology due to unsuccessful endodontic treatments. (B ) Extraction of teeth, placement of immediate implants and filling of socket cavities with guided bone regeneration (1st postoperative week). (C ) Postoperative 5th month panoramic radiograph image. (D ) Follow-up radiograph at 12 months after completion of prosthetic restorations
Source: Çolak S, Demïrsoy MS. Retrospective analysis of dental implants immediately placed in extraction sockets with periapical pathology: immediate implant placement in infected areas.
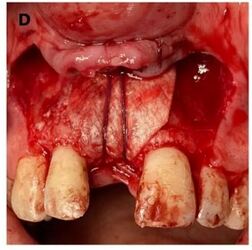
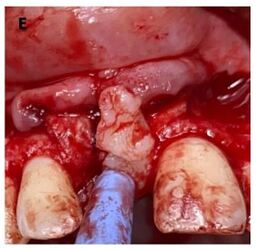
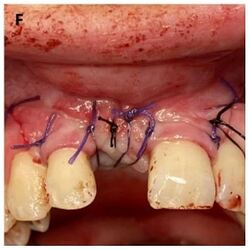
(A ) Radiographic view of the right maxillary central tooth with periapical pathology. (B ) Extraction socket after tooth extraction and curettage of periapical lesions. (C ) Immediate implant placement and grafting of the area. (D ) Covering the area with a membrane and securing it with a resorbable suture. (E ) Flipping the flap from the palatal mucosa. (F ) Primary closure of the area. (G ) Postoperative radiography
Source: Çolak S, Demïrsoy MS. Retrospective analysis of dental implants immediately placed in extraction sockets with periapical pathology: immediate implant placement in infected areas.
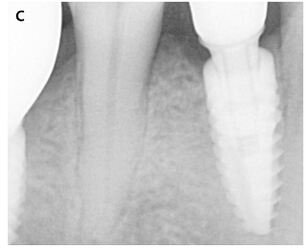
(A ) Right mandibular first premolar with periapical pathology. (B ) Placement of the implant after tooth extraction and curettage of the socket. (C ) Periapical radiography after completion of prosthetic restoration. (D ) 18. Monthly control radiograph
Source: Çolak S, Demïrsoy MS. Retrospective analysis of dental implants immediately placed in extraction sockets with periapical pathology: immediate implant placement in infected areas.
Key Point about Infected Sites
The key point summary is that: Studies have shown that the survival rates of implants placed in infected sites can be comparable to those placed in non-infected sites, as long as the correct protocols are followed. This includes, but is not limited to, thorough debridement of the infected site (some studies used laser laser decontamination, or ultrasonics), and use of standard guided bone regeneration (GBR) techniques. 1,2,3,4,5 .
References
1. Single Tooth Immediate Extraction Placement and Provisionalization in the Esthetic Area: Infected vs. Non-Infected Sites. A 2-To-12 Year Retrospective Clinical Study., Francesco Amato , Gazelle Jean Crasto , Giorgio Alfredo Spedicato , Dennis Tarnow , The International journal of oral & maxillofacial implants. Volume: 0, Issue: 0, 2025
PURPOSE
The aim of this study was to investigate and compare the survival rate and the success rate of single tooth implants placed and restored immediately after extraction in non-infected, acutely infected, and chronically infected sites in the maxillary anterior area.
MATERIAL AND METHODS
Patients requiring single tooth replacement of a maxillary central incisor, lateral incisor, canine, and premolar regions were included in the study. Implant sites were divided into three groups based on the presence or absence of an infection: Group 1 (Control) non-infected sites (healthy periodontal and endodontic conditions); Group 2 (Test 1) acutely infected sites (presence of a periodontal or endodontic or combined abscess and/or fistula); Group 3 (Test 2) chronically infected sites ( presence of a periodontal pocket or a periapical lesion with no signs of acute inflamation). The protocol applied required: flapless extraction, thorough debridement of the alveolus, immediate placement of the implant, particulate graft material insertion around the implant, resorbable membrane insertion in the facial aspect of the implant for all those cases in which the buccal plate was compromised, and immediate insertion of a screw-retained provisional FDP out of occlusion. The following parameters were evaluated: Periodontal and Endodontic initial conditions: gingival recession, probing depth, presence of an abscess and/or a fistula, extraction reason, presence of a periapical lesion, alveolar buccal wall integrity, distance between the gingival margin and the alveolar bone crest at mid-buccal, and implant insertion torque. Implant conditions at the last follow up included survival rate and marginal bone loss. Periodontal conditions: recession, probing depth, and gingival index. Final esthetic results: pink esthetic score. Statistical analysis was also performed.
RESULTS
After a mean follow-up of 7 years (range 2 to 12 years), a total of 127 patients were treated, 143 single tooth implants were placed and immediately restored with a provisional FDP: 47 implants in Group 1 control (non-infected sites), 56 implants in Group 2 Test 1 (acutely infected sites), 40 implants in Group 3 Test 2 (chronically infected sites). A survival rate of 97.8% for Group 1, 96.4% for Group 2, and 95% for Group 3 were recorded with no statistical difference between groups (p-value 0.8). A total of 5 implants failed, one in Group 1, two in Group 2, and two in Group 3 resulting in a cumulative implant survival rate of 96.5%.
CONCLUSIONS
The results of this study showed comparable implant survival rate between single tooth implants placed and restored immediately in a non-infected, acutely infected or chronically infected site. Read More
2. Retrospective analysis of dental implants immediately placed in extraction sockets with periapical pathology: immediate implant placement in infected areas., Sefa Çolak , Mustafa Sami Demïrsoy , BMC oral health. Volume: 23, Issue: 1, 2023
BACKGROUND
The aim of this study is to examine the survival rates of immediate implants placed in extraction sockets with chronic periapical pathology.
METHODS
69 patients and 124 immediate implants were included in the study. The patients included in the study were examined in 3 groups. Group 1: Patients who underwent tooth extraction with periapical pathology and immediate implant placement. Group 2: patients who underwent tooth extraction with periapical pathology, immediate implant placement and guided bone regeneration. Group 3: Patients who underwent tooth extraction with periapical pathology, sinus lift procedure and immediate implant placement. In statistical analysis, t-test and Anova analysis were used in the evaluation of quantitative data, cross-tables and chi-square (χ2) test were used in the evaluation of classified qualitative data. Statistical significance was determined as p < 0.05.
RESULTS
It was observed that 116 (95.55%) of 124 implants were successful and 8 (4.45%) failed. The success rate was 97.2% in Group 1, 93.5% in Group 2 and 81.8% in Group 3. A significant correlation was found between the study groups and implant success in terms of χ2 test (p = 0.037). A significant relationship was found between smoking and success in terms of the χ2 test (p = 0.015).
CONCLUSIONS
High survival rates are observed for immediate implant placement in sockets with periapical pathology. The success rates observed in guided bone regenerations simultaneously with immediate implant placement are at satisfactory levels. In cases where simultaneous sinus lifting procedures are required, the success rates were observed to be significantly lower. In case of adequate curettage and debridement in sockets with periapical pathology, high implant survival rates are observed. As the complexity of the surgical procedure increases, treatment protocols may progress in safer ways. Read More
3. Post-extraction implant placement into infected versus non-infected sites: A multicenter retrospective clinical study., Francesco Zuffetti , Matteo Capelli , Fabio Galli , Massimo Del Fabbro , Tiziano Testori , Clinical implant dentistry and related research. Volume: 19, Issue: 5, 2017
PURPOSE
The aim of this study was to assess whether immediate implant placement into post-extraction sites presenting a chronic infection poses a greater risk of implant failure than immediate placement in non-infected sites.
MATERIALS AND METHODS
Records of patients who underwent extraction and immediate implant placement into both infected and non-infected sites from January 1998 to September 2014 at 5 different dental centers were considered for inclusion. Included records were subjected to statistical analysis of survival rates, along with a number of other patient-, implant-, surgery-, and prosthesis-related variables.
RESULTS
The inclusion criteria were met by 369 patients who received a total of 527 implants. The follow-up averaged 53.2 months (range 0.9-158.3) for implants placed into non-infected sockets (N = 334) and 50.1 months (range 1.6-146.1) for those placed into infected sites (N = 193). Seven implants failed in non-infected sites and 3 in infected ones. All failures occurred within 1 year of placement. Cumulative implant survival rate for non-infected and infected sites was, respectively, 97.9% ± 0.8% and 98.4% ± 0.9%, being not significantly different (P = .66). None of the investigated variables affected the outcome.
CONCLUSIONS
Placement of implants into periodontally or endodontically infected sites immediately after tooth extraction is a safe option, even when the implants are loaded immediately or early. Read More
4. Immediate Implant Placement in Infected Sockets: A Consecutive Cohort Study., Ashish Kakar , Kanupriya Kakar , Minas D Leventis , Gaurav Jain , Journal of lasers in medical sciences. Volume: 11, Issue: 2, 2020 Spring
Immediate placement of implants in a fresh post-extraction socket is an increasingly popular and established treatment option. However, active infection in the extraction site may adversely affect the outcome of this procedure. This study was designed to assess the clinical results of immediate placement of dental implants in infected extraction sockets using a standardized protocol, which included () the use of an Er,Cr:YSGG laser for the decontamination of the infected socket prior to implant insertion, and () the utilization of an in situ hardening alloplastic bone graft substitute to augment the gap between the implant surface and the labial plate of bone. A retrospective record review was used to identify 68 patients who had implants placed as per the described protocol. A total of 126 implants were placed in 68 patients (65 implants in the maxilla, 61 implants in the mandible). The implants were loaded 136 ± 73 days (mean ± standard deviation; range: 37-400 days) after implant placement. Eight patients (16 implants) were subsequently lost to follow up. 105 of the 110 implants (95.45%) placed immediately in the infected sites using the described protocol survived after prosthetic loading. Immediate implant placement in previously infected sites using the protocols mentioned in our study with laser decontamination of the socket, grafting with an in situ hardening alloplastic bone graft material and non-submerged healing shows a similar survival rate to the published success rates for immediate implants placed in non-infected sites. Read More5. Immediate implants placed in infected and noninfected sites after atraumatic tooth extraction and placement with ultrasonic bone surgery., Cornelio Blus , Serge Szmukler-Moncler , Paul Khoury , Germano Orrù , Clinical implant dentistry and related research. Volume: 17 Suppl 1, Issue: , 2015
BACKGROUND
Only a few reports deal with implants placed in infected postextraction sites.
PURPOSE
Survival rates of a cohort of immediate implants cases placed in acute and chronically infected sites were compared with a cohort of noninfected ones while (1) tooth extraction and osteotomy sites were prepared with a piezosurgery device and (2) ultrasonication was applied to abate the bacterial charge at infected sites.
MATERIALS AND METHODS
Eighty-six patients received 168 immediate implants distributed into three groups: noninfected (85), acute (36), and chronically (47) infected sites. Atraumatic extraction and implant osteotomy were performed with an ultrasonic surgery device without flap elevation. All sites received the same medication and surgical protocol; infected sites were ultrasonicated during 30 seconds at 72 W. Kaplan-Meyer survival rates were calculated at 1 year.
RESULTS
The 1-year survival rates of the noninfected, chronically, and acute infected groups were 98.8, 100, and 94.4%, respectively. The differences were not statistically significant. No implant was lost after loading. All teeth and roots could be extracted in one piece. Drilling at extraction sockets was uncomplicated, without skidding.
CONCLUSIONS
Implant survival rates might be similar in infected and noninfected sites when infected sites receive standard medical and surgical treatment and are ultrasonicated. Atraumatic tooth/root extraction and implant placement can be reliably performed with piezoelectric surgery. Read More