This Week in Dental Implants we are tackling the following issues:
Can PRF membranes be improved thru the use of heat and used instead of collagen membranes or PTFE membranes? Additionally, what strategies are available for enhancing the long-term stability of Overdentures? Are certain Implant placement strategies better, and what are the effects of delayed vs immediate placement?
Quick PRF Background: What is Extended PRF?
The issue with regular PRF membranes has been that they resorb much too quickly. Extended PRF (e‑PRF) aims to solve that problem by heating the membrane with a proprietary machine called Bio‑Heat. The modification from the Bio-Heat machine slows the membrane’s resorption dramatically—extending its lifespan from the usual 2–3 weeks to roughly 4–6 months. The e‑PRF membrane canthen be used alone as a barrier membrane (instead of collagen or PTFE membranes) for ridge‑preservation procedures.
e-PRF Study
e-PRF with Xenograft for Immediate Implants in Aesthetic Zone -A Case Series.
- Group I (e‑PRF + xenograft): Showed significant improvements in pocket probing depth, tissue biotype, and bone volume.
- Group II (xenograft alone): Exhibited only minimal changes in probing depth, tissue biotype, and bone volume.
Combining e‑PRF with xenograft around immediate implants in the aesthetic zone leads to favorable hard‑ and soft‑tissue preservation, increased bone volume, and enhanced wound healing. e‑PRF appears to be a promising adjunct for immediate implant placement. 1
Case: Extended‐PRF membrane for Ridge Preservation.
Case below by: Nathan E Estrin,Troy B Tran,Alan Rene Espinoza et al., Clinical and experimental dental research. Volume: 12, Issue: 1, 2026 Safety and Feasibility of Extended Platelet-Rich Fibrin as a Solo Barrier Membrane for Ridge Preservation: A Case Series.
- Patients: 22 individuals requiring extraction of a single posterior tooth.
- Procedure: Atraumatic extraction → socket grafted with “sticky bone” (bone allograft + standard PRF). The e‑PRF membrane was placed over the graft as the sole barrier (replacing collagen or PTFE membranes).
- Assessments: Cone‑beam CT immediately after extraction and at 3 months; ridge width measured 1, 3, 5 mm apical to the crest and buccal/lingual height dimensions at both time points; buccal bone thickness recorded at baseline.
Conclusions
- Using e‑PRF membranes instead of collagen membranes for ridge preservation is safe, predictable, and effective.
- The membrane can be fabricated at low cost and resorbs much more slowly (4–6 months) than standard PRF (≈2 weeks), providing prolonged barrier function.
- While promising, further randomized controlled trials are needed to compare soft‑tissue outcomes against conventional membranes.
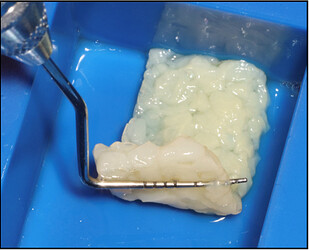
Figure 1.
Clinical demonstration of the final extended‐PRF membrane ready to use for ridge preservation.
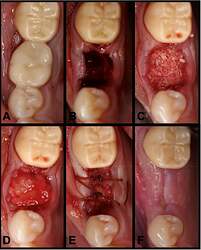
Figure 2.
(A) Preoperative clinical photograph. (B) After extraction of tooth #30, the socket was degranulated with a spoon excavator leaving a socket with a buccal dehiscence present. (C) The extraction socket was grafted with “sticky bone.” (D) The e‐PRF membrane was then placed over the grafted socket and (E) sutured with 3‐0 chromic gut in mattress fashion. (F) The patient was brought back for a 2‐week postoperative evaluation. Note the excellent healing and near complete wound closure.
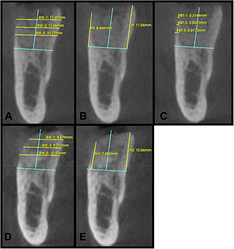
Figure 3.
A clinical case of ridge preservation at site #30 demonstrating radiographic measurements. (A) Baseline measurements of ridge width at 1 mm (RW‐1), 3 mm (RW‐3), and 5 mm (RW‐5) apical to the crest. (B) Baseline measurements of Buccal height (BH) and Lingual Height (LH). (C) Baseline buccal bone thickness at 1 mm (BBT‐1), 3 mm (BBT‐3), and 5 mm (BBT‐5) apical to the crest. (D) 3‐month postoperative ridge width measurements at all levels and (E) 3‐month postoperative buccal and lingual height measurements. All measurements were taken with the same vertical and horizontal reference lines (in blue) at both time intervals.
Enhancing the long-term stability of Overdentures
Study: Immediate vs Delayed?
Immediate and delayed loading protocols provide similar long‑term outcomes in terms of implant survival, clinical performance, radiographic bone levels, and patient‑reported comfort and satisfaction for two non‑splinted, locator‑retained mandibular overdentures. Immediate loading can be considered a reliable and potentially favorable option in appropriately selected cases, but regular recall and prosthetic maintenance are essential due to the high incidence of prosthetic complications.
Case: Implant Placement Strategies for Maxillary Implant‐Retained Overdenture
Case below by: Zahra Ghorbani,Ebrahim Shojaei,Hamid Neshandar Asli et al. Influence of Various Implant Placement Strategies on Stress Distribution in Maxillary Implant-Retained Overdenture: A 3D Finite-Element Analysis.
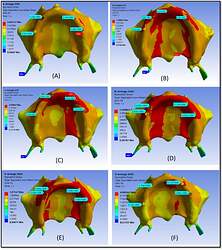
- Objective: To evaluate how different implant placement strategies affect the biomechanical behavior of maxillary implant‑supported overdentures using three‑dimensional finite‑element analysis (3‑D FEA).
- Conclusions
- A symmetrical implant arrangement (5R‑3R‑3L‑5L) offers the most favorable, uniform stress distribution, which may help preserve peri‑implant bone and enhance long‑term stability.
- Prioritizing implantation in the canine region is advisable.
- Mesially (more anterior) positioned implants in otherwise symmetrical layouts warrant caution because they generate higher stress levels.
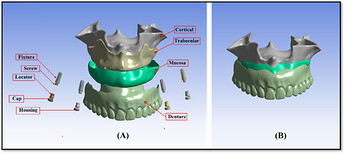
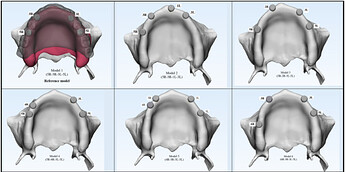
Figure 1.
Model geometry development: (A) All individual components of the overdenture system are shown separately. Each component is displayed in its actual spatial orientation to illustrate the detailed geometry and interaction surfaces before assembly. (B) The finite element model after assembly, showing all components integrated into one single, cohesive system. This assembled model represents the final configuration used for finite element analysis.
Figure 2.
Schematic representation of six models of implant placement strategies.
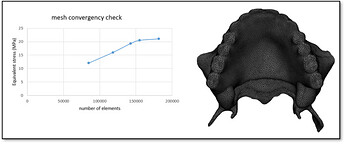
Figure 3.
Mesh sensitivity test. This figure illustrates the results of the mesh sensitivity test conducted to ensure the accuracy and reliability of the finite element simulations. Different mesh densities were applied to the reference and asymmetrical models, and the effect on maximum principal stress values in the bone was evaluated. The analysis confirmed that a mesh configuration with a maximum of 5% error was sufficient to capture stress distribution patterns accurately, balancing computational efficiency and result precision. By performing this test, we ensured that the selected element size and node distribution did not significantly influence the simulation outcomes, providing confidence that the stress predictions reflect the true biomechanical behavior of the overdenture‐implant system.
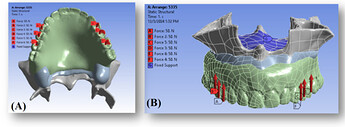
Figure 4.
(A) An occlusal load of 300 N was applied bilaterally on the premolars and first molars (150 N per side) to simulate masticatory forces. (B) The surfaces constrained in all degrees of freedom are highlighted with blue dots, representing the fixed boundary conditions applied to the maxillary bone to prevent rigid body motion during simulation. These constraints ensure numerical stability and allow accurate calculation of stress distribution within the implant‐supported overdenture system.
Figure 5.
Stress distribution patterns in cortical bone across the six overdenture models based on the von Mises criterion. Each panel represents a different implant placement configuration: (A) Model 1 (5R–3R–3L–5L), (B) Model 2 (5R–3R–1L–3L), (C) Model 3 (5R–2R–3L–5L), (D) Model 4 (5R–4R–3L–5L), (E) Model 5 (4R–3R–3L–5L), and (F) Model 6 (6R–3R–3L–5L).The color scale indicates the magnitude of maximum principal stress in cortical bone, ranging from low stress (blue) to high stress (red). This qualitative visualization enables comparison of stress concentration patterns among the models. The reference model (A) exhibits a more uniform stress distribution, whereas certain asymmetrical configurations show localized stress peaks, highlighting areas at higher risk of overload and demonstrating the influence of implant position on biomechanical performance and bone preservation.
References
-
Safety and Feasibility of Extended Platelet-Rich Fibrin as a Solo Barrier Membrane for Ridge Preservation: A Case Series.
Nathan E Estrin,Troy B Tran,Alan Rene Espinoza et al., Clinical and experimental dental research. Volume: 12, Issue: 1, 2026
Platelet-rich fibrin (PRF) has been commonly utilized for ridge preservation techniques… -
Influence of Various Implant Placement Strategies on Stress Distribution in Maxillary Implant-Retained Overdenture: A 3D Finite-Element Analysis.
Zahra Ghorbani,Ebrahim Shojaei,Hamid Neshandar Asli et al., Clinical and experimental dental research. Volume: 12, Issue: 1, 2026
This study used three-dimensional (3D) finite-element analysis (FEA) to investigate the effect of different implant placeme… -
e-PRF with Xenograft for Immediate Implants in Aesthetic Zone -A Case Series.
Sai Vinitha B,Vinaya Rudresh,Prabhuji Mlv et al., The International journal of oral & maxillofacial implants. Volume: 0, Issue: 0, 2026
The aim of this novel study was to assess the effects of e-PRF (Extended PRF) along with xenograft and xenograft alone around … -
Immediate versus Delayed Loading of Mandibular Implant Retained Overdentures: A 12 Year Follow-up of a Randomized Clinical Trial.
Jennifer Duffy,Ajay Dhingra,Satoko Ono Rubin et al., The International journal of oral & maxillofacial implants. Volume: 0, Issue: 0, 2026
The purpose of this prospective 12-year long-term follow-up of a randomized clinical trial was to evaluate clinical and radiog…