While the success rate of dental implants remains very high, unfortunately some do fail. In this post, we review the basic causes of failure, as well as the accepted techniques for removing failed implants. The quick summary: For late failures where removal is indicated, use the reverse torque technique or a combination technique to remove the implant.
Implant Removal Kit
The implant removal kit contains the tools you need to remove a failed dental implant while minimizing trauma to the bone.
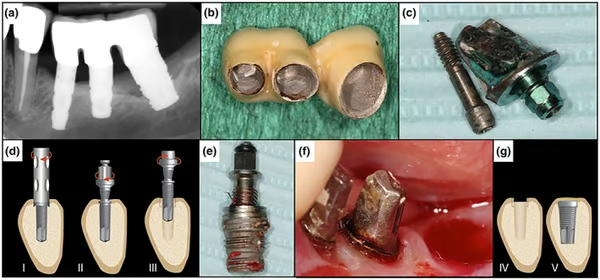
Case Photos
(a) Preoperative X‐ray showing advanced peri‐implantitis in Region 38. (b) Removal of the temporary cemented three‐piece bridge. (c) Disconnection of the abutment. (d) (I) If needed, a trephine bur is used to remove the first 2 cm of bone‐to‐implant contact (in this case not needed); (II) the screw is applied and cut counterclockwise into the implant; (III) counterclockwise torque is applied until the implant becomes loose and is unwinded. (e) Removed implant from Region 38. (f) Post‐operation site. (g) (IV) The socket has been kept in good condition and ready for regeneration and/or for a new implant (V) (as described by Anitua and Orive, 2012)
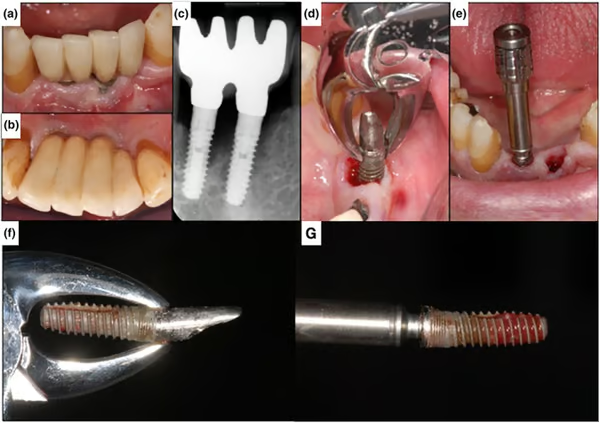
(a,b) Preoperative clinical situation. (c) X‐ray. Arrows showing the bone defect depth (d). Removal of the implant (c,f) with a forceps by counterclockwise rotation. (e) Implant removal (c,g) with the reverse screw technique. Arrows showing height of previous bone level. (f,g) Showing both implants after removal. Arrows showing height of previous bone level
Source: Solderer A, Al-Jazrawi A, Sahrmann P, Jung R, Attin T, Schmidlin PR. Removal of failed dental implants revisited: Questions and answers. Clin Exp Dent Res. 2019
Implant Failure Distinction: Early vs. Late
When it comes to implant failure it is useful to distinguish between early failure and later failure. Early failures, within the first few weeks or months after implant placement, happen before the implants are fully loaded and typically reflect insufficient healing and osseointegration during the initial phase. The reported prevalence of early implant-level failure varies across a wide range. Please see the references below for additional data.
Late failure refers to failure that occurs after osseointegration and functional loading with prosthetics, meaning it happens once osseointegration is complete. The reported prevalence of late failure at the implant level also has a wide range and is dependent on many factors. Please consult the references below for additional data.
Reasons for Early Failure
Early implant failures are generally caused by patient-specific factors, and sometimes more importantly clinical mistakes due to a lack of surgical experience. Patient related factors include: smoking, diabetes, radiotherapy, bone quality (early implant failure was more likely to occur in the sparse bone types) and potential allergic reactions to titanium (Ti allergy can be detected in dental implant patients, even though its estimated prevalence is low (0.6%)). With regards to surgical reasons for implant failure, the main issues are generally, overheating of the bone during preparation of the implant site, lack of primary stability due to overpreparation of the implant site or poor bone quality, and improper insertion or flap techniques.
Etiology of Late Failure
The two primary causes of late failure of dental implants are peri‐implantitis and implant fractures. Secondary causes are medication (many studies have reported medication-related osteonecrosis of the jaw with patients on bisphosphonate treatment), and implant malpositioning (ncorrectly positioned implants can cause functional or esthetic complications). With regards to peri‐implantitis, some studies have shown that occurs in approximately 28% to 77% of patients and in 12% to 43% of implants. Implant fracture is a bit of a more complicated topic with the prevalence very closely aligned with the type of implant placed, e.g. fracture rates reported of 3.5% of internal connection implants over 14 years. In addition patients with bruxism may show higher rates of fractures, so with bruxers nightguards might provide some degree of protection.
Removal of Failed Implants?
Luckily in early implant failure, the implant is generally always mobile so removal is indicated and is easily achieved. Late failure is much more complicated since the implants are osseointegrated and not mobile. The decision to remove an implant at a later date is subject to the cause. Fractured implants obviously need to be removed, but periimplantitis is not necessarily a reason to remove an implant and various criteria have been offered for this situation. Misch et al. recommended the removal of nonmobile implants with 50% bone loss as failures, while Greenstein et al. recommended the removal of implants with ≥ 75% bone resorption or ≤ 3-mm apical bone around the implants. Surgical therapy for peri-implantitis has a very poor prognosis when there is severe bone loss.
Removal Techniques
In terms of implant removal techniques for later stage failures where the implant is non-mobile, there are several recommended options:
- Counter-torque Technique: Recommended Option
In the counter or reverse torque technique, a reverse-threaded screw is driven counterclockwise into the damaged implant. The special threading of the screw allows engagement with the failed implant. Then using a special wrench, a counter‐torque‐wise force is applied to remove the implant. The Implant Removal Kit provides all the tools needed for the reverse torque technique. It should be noted, however, that the reverse torque technique is not recommended when the torque required may exceed 200 ncm. In those cases, the suggested solution is to use a combination technique. First use a bone‐cutting method, as trephine burs or piezo, to remove the surrounding 3–4 mm of bone, and then use the reverse torque technique to remove the implant.
- Burs and Piezosurgery: \ In this technique, the implant is gradually removed using burs, forceps, and piezosurgery. Piezosurgery allows bone cutting while preventing soft tissue damage. However, this technique requires significant skill and experience, since the heat generated by piezo can cause issues. For example, physiological saline must be injected at various points to prevent overheating of the tip.
- Trephines: Trephines are a popular option for removing failed implants, but they come with a risk of significant damage to the surrounding bone. As such, they should always be a last resort. In general, as explained above, they are best used in combination with the reverse torque technique, when the implants are too osseointegrated to be removed by reverse torque alone.
References
Treatment strategies for dental implant removal: A literature review Jpn Dent Sci Rev. 2024 Feb 23;60:120–127. - Masaki C, Kondo Y, Tomoeda K, Nodai T, Munemasa T, Mukaibo T, Hosokawa R.
Various tools have been developed to facilitate implant removal, bringing great benefit to both patients and dentists. Because implant removal with a trephine bur results in a large defect in the surrounding bone, minimally invasive procedures for implant removal using the reverse torque technique are the first treatment choice. Implant problems can be solved temporarily by implant removal. However, for subsequent prosthetic treatment, the patient's age and general condition and retreatment costs should be considered, and a new treatment plan should be established after the causes of the problems are determined. Therefore, we should evaluate the cause of the problem, such as diabetes, smoking, or overloading, to see if it can be resolved before proceeding with reimplantation or considering a change to a removable denture. In this review, we have summarized the current research regarding implant removal and reimplantation; however, it is clear that insufficient evidence is available and further research is required in this field.Read MoreRemoval of failed dental implants revisited: Questions and answers, Clin Exp Dent Res. 2019 Aug 21;5(6):712–724. - Solderer A, Al-Jazrawi A, Sahrmann P, Jung R, Attin T, Schmidlin PR.
Early and late implant failure normally have different causes and can be treated in different ways.Peri‐implantitis shows to be the main reason for late implant failure.
Trephine burs seem to be the best‐known method for implant removal.
The CTRT method alone or combined, because of the low invasiveness, should be the first choice for the clinician.
Scarce data regarding zirconia implant removal are available. Because of zirconia’s physical properties, it is supposed that they require a different approach compared with titanium implants.
The defect type of the bone at the failed implant is crucial for the choice of the removal method and the subsequent treatment.
Implantation in previously failed sites irrespective of an early or late failure results in 71% to 100% survival after an average of 69.4 months.Read More