Sufficient gingival tissue surrounding dental implants is considered important for both functional and aesthetic purposes. There are many soft tissue grafting techniques that have been proposed that aim to improve soft tissue and achieve an adequate width of keratinized tissue (KT). The Free Gingival Graft (FGG) is a surgical procedure used to augment the amount of keratinized mucosa. It involves harvesting a piece of tissue from the palate and transplanting it to the area where additional keratinized tissue is needed. There are drawbacks to the FGG procedure, and other graft alternatives, including acellular dermal matrix (ADM) and collagen sponges, have also been proposed for soft tissue grafting. Below are the top 10 cited research articles on FGG, to aid you in further research on this important topics, followed by a quick case demonstrating the use of DALI Acellular Dermis (ADM) as an option for buccal contour augmentation around implants (scroll down to see the case).
The Top 10 Articles on FGG
Efficacy of periodontal plastic surgery procedures in the treatment of localized facial gingival recessions. A systematic review., Francesco Cairo , Michele Nieri , Umberto Pagliaro , Journal of clinical periodontology. Volume: 41 Suppl 15, Issue: , 2014
Fifty-one RCTs (53 articles) with a total of 1574 treated patients (1744 recessions) were included in this SR. Finally, 30 groups of comparisons were identified and a total of 80 meta-analyses were performed. Coronally Advanced Flap (CAF) was associated with higher probability of CRC and higher amount of RecRed than Semilunar Coronal Positioned Flap (SCPF). The combination CAF plus Connective Tissue Graft (CAF+CTG) or CAF plus Enamel Matrix Derivative (CAF+EMD) was more effective than CAF alone in terms of CRC and RecRed. The combination CAF plus Collagen Matrix (CAF+CM) achieved higher RecRed than CAF alone. In addition, CAF+CTG achieved CRC more frequently than CAF+EMD, SCPF, Free Gingival Graft (FGG) and Laterally Positioned Flap (LPS). CAF+CTG was also associated with higher RecRed than Barrier Membranes (CAF+GTR), CAF+EMD and CAF+CM. GTR was not able to improve the clinical efficacy of CAF. Studies adding Acellular Dermal Matrix (ADM) under CAF showed a large heterogeneity and not significant benefits compared with CAF alone. Multiple combinations, using more than a single graft/biomaterial under the flap, usually provide similar or less benefits than simpler, control procedures in term of root coverage outcomes. CAF procedures alone or with CTG, EMD are supported by large evidence in modern periodontal plastic surgery. CAF+CTG achieved the best clinical outcomes in single gingival recessions with or without iCAL. Read MoreTissue alterations after tooth extraction with and without surgical trauma: a volumetric study in the beagle dog., Stefan Fickl , Otto Zuhr , Hannes Wachtel , Wolfgang Bolz , Markus Huerzeler , Journal of clinical periodontology. Volume: 35, Issue: 4, 2008
The aim of this study is to evaluate whether tooth extraction without the elevation of a muco-periosteal flap has advantageous effects on the resorption rate after tooth extraction.RESULTS The “flapless groups” demonstrated significant lower resorption rates both when using socket-preservation techniques and without. Furthermore, socket-preservation techniques yielded better results compared with not treating the socket.
CONCLUSION The results demonstrate that leaving the periosteum in place decreases the resorption rate of the extraction socket. Furthermore, the treatment of the extraction socket with BioOss Collagen and a free gingival graft seems beneficial in limiting the resorption process after tooth extraction.
Efficacy of soft tissue augmentation around dental implants and in partially edentulous areas: a systematic review., Daniel S Thoma , Borvornwut Buranawat , Christoph H F Hämmerle , Ulrike Held , Ronald E Jung , Journal of clinical periodontology. Volume: 41 Suppl 15, Issue: , 2014
Nine (KM) and eleven (volume) studies met the inclusion criteria. An apically positioned flap/vestibuloplasty (APF/V) plus a graft material [free gingival graft (FGG)/subepithelial connective tissue graft (SCTG)/collagen matrix (CM)] resulted in an increase of keratinized tissue (1.4-3.3 mm). Statistically significantly better outcomes were obtained for APF/V plus FGG/SCTG compared with controls (APF/V alone; no treatment) (p < 0.05). For surgery time and patient morbidity, statistically significantly more favourable outcomes were reported for CM compared to SCTGs (p < 0.05) in two randomized controlled clinical trials (RCTs), even though rendering less keratinized tissue. SCTGs were the best-documented method for gain of soft tissue volume at implant sites and partially edentulous sites. Aesthetically at immediate implant sites, better papilla fill and higher marginal mucosal levels were obtained using SCTGs compared to non-grafted sites. An APF/V plus FGG/SCTG was the best-documented and most successful method to increase the width of KM. APF/V plus CM demonstrated less gain in KM, but also less patient morbidity and surgery time compared to APF/V plus SCTG based on two RCTs. Autogenous grafts (SCTG) rendered an increase in soft tissue thickness and better aesthetics compared to non-grafted sites. Read MoreAutogenous soft tissue grafting for periodontal and peri-implant plastic surgical reconstruction., Giovanni Zucchelli , Lorenzo Tavelli , Michael K McGuire , Giulio Rasperini , Stephen E Feinberg , Hom-Lay Wang , William V Giannobile , Journal of periodontology. Volume: 91, Issue: 1, 2020
This state-of-the-art review presents the latest evidence and the current status of autogenous soft tissue grafting for soft tissue augmentation and recession coverage at teeth and dental implant sites. The indications and predictability of the free gingival graft and connective tissue graft (CTG) techniques are highlighted, together with their expected clinical and esthetic outcomes. CTGs can be harvested from the maxillary tuberosity or from palate with different approaches that can have an impact on graft quality and patient morbidity. The influence of CTGs on soft tissue thickness and keratinized tissue width are also discussed. Read MoreKeratinized mucosa around implants in partially edentulous posterior mandible: 10-year results of a prospective comparative study., Mario Roccuzzo , Giancarlo Grasso , Paola Dalmasso , Clinical oral implants research. Volume: 27, Issue: 4, 2016
Ninety-eight patients completed the 10-year study. The absence of KT was associated with higher plaque accumulation, greater soft-tissue recession (REC), and a higher number of sites that required additional surgical and/or antibiotic treatment. Patient-reported outcomes regarding maintenance procedures presented major differences between the groups. In 11 of the 35 AM cases, additional free gingival graft (FGG) was successfully employed to reduce discomfort and to facilitate optimal plaque control. Implants that are not surrounded by KT are more prone to plaque accumulation and REC, even in patients exercising sufficient oral hygiene and receiving adequate supporting periodontal therapy (SPT). In selected cases, particularly in the edentulous posterior mandible, where ridge resorption leads to reduced vestibular depth and lack of KT, additional FGG can be beneficial to facilitate proper oral hygiene procedures. Read MorePeri-implant soft tissue phenotype modification and its impact on peri-implant health: A systematic review and network meta-analysis., Lorenzo Tavelli , Shayan Barootchi , Gustavo Avila-Ortiz , Istvan A Urban , William V Giannobile , Hom-Lay Wang , Journal of periodontology. Volume: 92, Issue: 1, 2021
The peri-implant soft tissue phenotype (PSP) encompasses the keratinized mucosa width (KMW), mucosal thickness (MT), and supracrestal tissue height (STH). Numerous approaches to augment soft tissue volume around endosseous dental implants have been investigated. To what extent PSP modification is beneficial for peri-implant health has been subject of debate in the field of implant dentistry. The aim of this systematic review was to analyze the evidence regarding the efficacy of soft tissue augmentation procedures aimed at modifying the PSP and their impact on peri-implant health.A total of 52 articles were included in the qualitative analysis, and 23 RCTs were included as part of the network meta-analysis. Sixteen RCTs reported the outcomes of PSP modification therapy with bilaminar techniques, whereas 7 involved the use of APF. The analysis showed that bilaminar techniques in combination with soft tissue grafts (connective tissue graft [CTG], collagen matrix [CM], and acellular dermal matrix [ADM]) resulted in a significant increase in MT compared to non-augmented sites. In particular, CTG and ADM were associated with higher MT gain as compared to CM and non-augmented sites. However, no significant differences in KMW were observed across different bilaminar techniques. PSP modification via a bilaminar approach utilizing either CTG or CM showed beneficial effects on marginal bone level stability. APF-based approaches in combination with free gingival graft (FGG), CTG, CM, or ADM showed a significant KMW gain compared to non-augmented sites. However, compared to APF alone, only FGG exhibited a significantly higher KMW gain. APF with any evaluated soft tissue graft was associated with with reduction of probing depth, soft tissue dehiscence and plaque index compared to non-augmented sites compared to non-augmented sites.
The evidence regarding the effect of PSP modification via APF-based approaches on peri-implant marginal bone loss or preservation is inconclusive. Bilaminar approach involving CTG or ADM obtained the highest amount of MT gain, whereas APF in combination with FGG was the most effective technique for increasing KMW. KMW augmentation via APF was associated with a significant reduction in probing depth, soft tissue dehiscence and plaque index, regardless of the soft tissue grafting material employed, whereas bilaminar techniques with CTG or CM showed beneficial effects on marginal bone level stability.
Read More
The connective tissue graft: a comparative clinical evaluation of wound healing at the palatal donor site. A preliminary study., Massimo Del Pizzo , Fabio Modica , Nicola Bethaz , Patrik Priotto , Roberto Romagnoli , Journal of clinical periodontology. Volume: 29, Issue: 9, 2002
The aim of this study is to evaluate early healing results of the palatal wound by comparing three different surgical procedures for harvesting a connective tissue graft: the single-incision (SI), the free gingival graft (FGG) and the trap-door (TD) techniques.Statistically significant differences were found between the SI and FGG techniques in terms of CE, which occurred faster in the SI group. The discomfort rate recorded for both SI and TD groups was significantly lower than for FGG group. No marked differences were noted between SI and TD procedures. The latter was confirmed by patient interviews. The results of this preliminary study have little statistical significance because of the limited number of patients but they represent an important basis for a comparative clinical study, with a larger sample of participants, which is currently in progress. Read MorePatient outcomes following subepithelial connective tissue graft and free gingival graft procedures., Jeffrey R Wessel , Dimitris N Tatakis , Journal of periodontology. Volume: 79, Issue: 3, 2008
|Subepithelial connective tissue grafts (CTGs) and free gingival grafts (FGGs) are common periodontal procedures with similar indications; however, they may differ regarding patient outcomes. Reports on postoperative periodontal patient outcomes are limited. The aim of this observational trial was to compare patient-based outcomes for CTGs and FGGs. Twenty-three subjects (12 CTGs and 11 FGGs) completed the study. Differences between CTG and FGG groups in VAS pain scores at 3 days did not reach statistical significance. The proportion of subjects reporting pain in the palate at 3 days was significantly greater for FGG (P <0.05). There were no significant intergroup differences at 3 weeks. For the FGG group, 3-week VAS pain scores were less than the 3-day ones (P <0.01). For the entire study population, the number of days analgesic pills were taken, total number of analgesic pills taken, and number of pills taken from day 3 to the end of the study correlated with the 3-week pain scores.FGG is associated with a greater incidence of donor site pain compared to CTG at the early postoperative period. Longer-term pain after soft tissue grafting is associated with greater analgesic usage. There is an opportunity to improve the postoperative protocols of soft tissue grafting, particularly for FGG. :::| Read MoreEvidence-based mucogingival therapy. Part 2: Ordinary and individual patient data meta-analyses of surgical treatment of recession using complete root coverage as the outcome variable., Carlo Clauser , Michele Nieri , Debora Franceschi , Umberto Pagliaro , Giovanpaolo Pini-Prato , Journal of periodontology. Volume: 74, Issue: 5, 2003
|The literature (1970-2000) on the outcome of surgical root coverage has been revised and summarized in a companion paper. The overall conclusion was that the various procedures are effective, but it was not possible to determine which procedure was best indicated in different clinical conditions. In this study, meta-analysis techniques were used to seek evidence for guiding clinical decisions when planning root coverage surgery. The aim of this study was to illustrate the differences between meta-analyses applied to summarized and individual patient data (IPD) and to present suggestions for reducing the costs of IPD meta-analysis. :The first analysis showed that CRC was achieved more often in non-randomized than in randomized studies. The heterogeneity tests revealed great variability of results in both the randomized and non-randomized studies, which makes it difficult to draw any definite conclusions. In the second analysis all the tested techniques revealed similar trends: greater baseline recession depths were always associated with a decreased CRC. The third analysis showed that CRC was achieved more frequently in the sites treated with CTG as opposed to GTR. The small sample size and the lack of IPD rendered the analyses inconclusive despite the randomized design. Few studies reported individual patient data; they are a valuable contribution to clinical decision making, but IPD published in the literature are still insufficient to provide a reliable guide for clinical decision making. Therefore, decisive steps should be taken to facilitate the publication of IPD, in electronic format, whenever a clinical study is published in a leading journal. :::| Read MoreAcellular dermal matrix allografts to achieve increased attached gingiva. Part 1. A clinical study., P C Wei , L Laurell , M Geivelis , M W Lingen , D Maddalozzo , Journal of periodontology. Volume: 71, Issue: 8, 2000
Freeze-dried acellular dermal matrix (ADM) allograft, originally used for full-thickness burn wounds, was recently introduced as an alternative to the autogenous free gingival graft (FGG) in achieving increased attached keratinized tissue. The aim of part 1 of this study was to investigate the clinical efficacy of the ADM allograft for this particular purpose. The results of this study suggest that in procedures aiming at increasing the width of attached gingiva: 1) the ADM allograft was less effective and less predictable than the autogenous FGG in terms of increasing attached keratinized tissue due to considerable shrinkage and inconsistent quality of the attached tissue gained and 2) the esthetic results using the ADM allograft might be better than those using the autogenous FGG. Read MoreAcellular dermal matrix allografts to achieve increased attached gingiva. Part 2. A histological comparative study., Pein-Chi Wei , Lars Laurell , Mark W Lingen , Milton Geivelis , Journal of periodontology. Volume: 73, Issue: 3, 2002
In part 1 of this study, we compared the clinical efficacy of freeze-dried acellular dermal matrix (ADM) allograft in 6 patients with autogenous free gingival graft (FGG) in 6 patients for increasing the width of attached gingiva in the mandibular anterior area. The purpose of the present study was to histologically compare the microstructure of ADM and FGG treated sites from the same group. The results of this 6-month histological evaluation suggest that: 1) the resultant tissue types of ADM grafts were similar to "scar" tissue; 2) the non-vital dermal matrix of ADM allograft lacked the capability of directing cyto-differentiation of the covering epithelium; 3) autogenous FGG-derived tissue was neither identical to donor palatal mucosa nor to adjacent gingiva propria; 4) the connective tissue of donor palatal mucosa only partially contributed to the differentiation of the epithelium covering the FGG-treated area; and 5) the epithelium/connective tissue microenvironment surrounding the recipient site influenced the epithelial differentiation of the graft; this may play a more critical role in ADM grafting than in the grafting of autogenous FGG. Read MoreClinical Cases: Improving Buccal Contour Augmentation with DALI Dermis
(Case Presented by: Dr. Daniel Gober, Marine Park Perio)
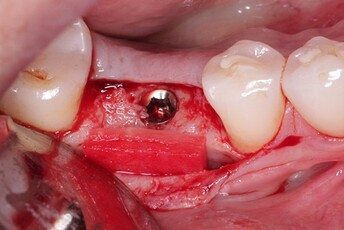
DALI Acellular Dermis (ADM) is a great option for buccal contour augmentation around implants at the time of placement and for increasing tissue thickness. Depending on the buccal bone thickness, it can be used with or without a bone graft.
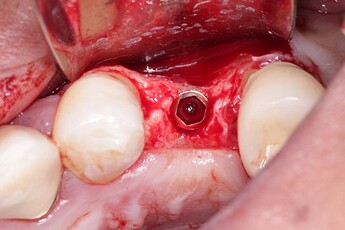
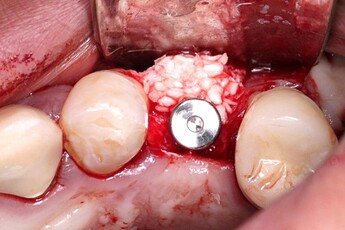
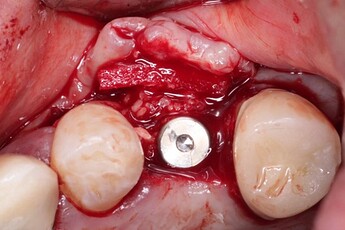
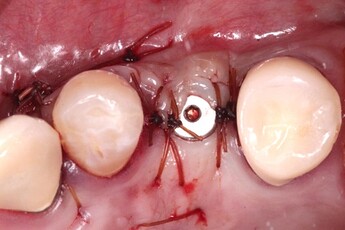
For example, site 12 presented with a significant buccal contour defect (1). Once the implant was placed (2), the site was augmented simultaneously with DALI Classic Bone Particulate and DALI Dermis ADM (3 & 4). DALI ADM was used instead of a membrane in order to add tissue thickness as well. The matrix is best applied dry to the site and then it will soak up blood from the site increasing its volume. As long as there is passive adaptation of the flap when sutured, healing is uneventful and increased contour can be achieved (5 & 6).
Alternatively, in another case, as shown, when the bone thickness is adequate (7 & 8). It can be used by itself to increase tissue thickness. Again, the matrix is placed dry and allowed to soak up blood from the area. It can also be double-layered for increased volume as long as passive flap adaptation is achieved (9 & 10). This simple technique can achieve a great increase in contour following healing (11)