This Week in Dental Implants we wanted to present a case which demonstrates, a unique, but highly effective way to enhance your GBR and ensure excellent surgical outcomes with the use of a DALI Amnion-Chorion membrane in a double-layer membrane technique. Let’s get right to the case. If you are interested in some additional research resources, please see the Case Discussion section below after the case.
Case Presentation
Case Presented By: Dr. Daniel Gober, Marine Park Perio
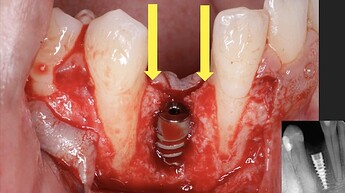
This case involved a missing #27, which was a previously failed implant site by another office. Another surgeon removed the implant and grafted the site (1). A flap was opened and revealed bone graft material that didn’t take. The entire site was cleaned out and we were left with the defect, as seen (2). An osteotomy was prepared and an implant was placed. We were optimistic about the success of the GBR, because there were nice bone peaks on adjacent teeth and the implant was well within the alveolar housing. GBR should be predictable in this case. (3,4).
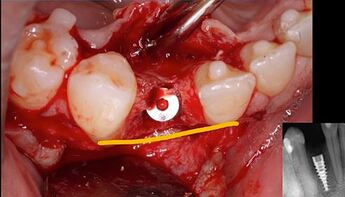
The GBR procedure proceeded in a standard fashion with the membrane tucked under the lingual flap, with bone graft (DALI Classic Mineralized Cortical Cancellous) added on top of around the implant (5). The membrane (OsseoSeal collagen membrane) was then placed over the bone and extending onto native bone. OsseoSeal was a great option for this case, because of how it contours around the graft material (6). Next, we employed the dual or double-layer membrane technique to enhance our healing by layering over the OsseoSeal collagen membrane with the DALI Amnion-Chorion Membrane. Remember, it’s really important to place the Amnion-Chorion membrane dry because when this membrane gets wet, it is extremely sticky and very difficult to manipulate (7). Finally, we suture the site and achieve primary closure using the periosteal releasing incisions and tension-relieving sutures sutures (8).
3 months later at post-op, we can see great soft tissue healing, an increase in ridge contour, and the implant is well integrated, while the bone graft healed, as well (9). The implant was then surgically uncovered and we encountered bone covering the implant. A was bur used to remove bone to gain access to cover screw. The restorative platform is revealed and was implant completely surrounded by bone, signaling a successful GBR procedure (10,11). The implant restored with a screw retained crown.(12).
When comparing the pre-op and post op (13), it’s clear that we were able to both place the implant and regenerate bone successfully, as well as get a really nice restoration. One side benefit of the procedure was that you will notice that some root coverage was achieved, as well on #28, even if that was not a primary goal of the procedure. Perhaps the DALI Amnion-Chorion membrane contributed to that additional beneficial outcome.
Case Discussion
The double layer membrane technique is a method used in guided bone regeneration (GBR) to enhance the efficacy of GBR. This technique generally involves using two layers of a collagen membrane to cover the grafted area. The purpose of the dual layer is to provide better protection via enhanced barrier function and improved stability to the graft, optimizing the regenerative area as compared to a single-layer membrane.
Several studies have investigated the double-layer membrane technique, and the results are not definitive. One animal study, concluded positively that:
“Furthermore, the double-layer technique using non-cross-linked collagen membranes (BioGide((R))) can enhance the efficacy of the onlay block bone graft technique in terms of both bone resorption and augmentation compared with a single-layer collagen membrane.” 1
However, a small study in patients, showed that:
“Within the limitations of this study, single-layer and double-layer coverage with collagen membranes after ARP failed to show substantial differences in the preservation of horizontal or vertical dimensions or in clinical healing.” 2
While the results for a double layer seem conflicting, the issue mainly seems to be that all the studies utilize only collagen membranes in the technique. However, the results could be enhanced by layering of amnion-chorion membrane on top of the collagen membrane, as suggested by Fien et al.:
“The use of a collagen membrane in combination with a dehydrated amnion/chorion membrane (dHACM) can facilitate stabilization of the bone graft and membrane by providing the benefits of a long-lasting bioabsorbable collagen membrane in addition to the unique benefits of an amnion/chorion membrane, which has been shown to provide growth factors to the surgical site that have potential to enhance regenerative outcomes.” 3
The use of Amnion/chorion membranes is supported by various studies 4,5,6,7,8,9 These membranes possess unique biological properties that improve wound healing and enhance regeneration. They have been used in treatments such as gingival recession, intrabony and furcation defect treatment, alveolar ridge preservation, and maxillary sinus membrane repair. The combination of amnion/chorion membranes with other materials, like bone grafts, has shown promising results in guided bone regeneration and tissue regeneration procedures. They provide growth factors to surgical sites, which can enhance regenerative outcomes. A list of some interesting studies are included below which can be used for further research.
References
1. The efficacy of a double-layer collagen membrane technique for overlaying block grafts in a rabbit calvarium model., Su-Hwan Kim , Do-Young Kim , Kyoung-Hwa Kim , Young Ku , In-Chul Rhyu , Yong-Moo Lee , Clinical oral implants research. Volume: 20, Issue: 10, 2009
OBJECTIVES
To analyze the outcomes of a single- and a double-layered collagen membrane on the efficacy of onlay block grafts in terms of bone resorption and augmentation.
MATERIAL AND METHODS
A total of 36 New Zealand white rabbits were used in this study. Calvarial bone blocks were obtained from one side of the parietal bone and fixed on the contaralateral side. The onlay grafts were covered with either no (C group), one (M1 group), or two (M2 group) layers of a non-cross-linked collagen membrane (BioGide((R))). After 2, 4, and 6 months of healing, rabbits were sacrificed and explanted specimens were prepared for histologic and histomorphometric analysis. At each period, the overall pattern of graft bone resorption and membrane biodegradation were examined histologically, and the sustained external form of grafted bone (%) and the remaining mineralized bone volume (%) were measured histomorphometrically.
RESULTS
The M1 and M2 groups exhibited decreased bone resorption compared with the C group at all periods. The M2 group had less graft resorption and a higher bone density of the grafted bone than the M1 group. In the M1 group, the collagen membrane was degraded partially or completely by 4 months and was absent at 6 months. Conversely, for the M2 group, the membrane body was retained up to 6 months.
CONCLUSIONS
Our results demonstrated that the collagen membrane used here can reduce graft bone resorption. Furthermore, the double-layer technique using non-cross-linked collagen membranes (BioGide((R))) can enhance the efficacy of the onlay block bone graft technique in terms of both bone resorption and augmentation compared with a single-layer collagen membrane. Read More
2. Alveolar ridge preservation with an open-healing approach using single-layer or double-layer coverage with collagen membranes., Ho-Keun Choi , Hag-Yeon Cho , Sung-Jo Lee , In-Woo Cho , Hyun-Seung Shin , Ki-Tae Koo , Hyun-Chang Lim , Jung-Chul Park , Journal of periodontal & implant science. Volume: 47, Issue: 6, 2017
PURPOSE
The aim of this prospective pilot study was to compare alveolar ridge preservation (ARP) procedures with open-healing approach using a single-layer and a double-layer coverage with collagen membranes using radiographic and clinical analyses.
METHODS
Eleven molars from 9 healthy patients requiring extraction of the maxillary or mandibular posterior teeth were included and allocated into 2 groups. After tooth extraction, deproteinized bovine bone mineral mixed with 10% collagen was grafted into the socket and covered either with a double-layer of resorbable non-cross-linked collagen membranes (DL group, n=6) or with a single-layer (SL group, n=5). Primary closure was not obtained. Cone-beam computed tomography images were taken immediately after the ARP procedure and after a healing period of 4 months before implant placement. Radiographic measurements were made of the width and height changes of the alveolar ridge.
RESULTS
All sites healed without any complications, and dental implants were placed at all operated sites with acceptable initial stability. The measurements showed that the reductions in width at the level 1 mm apical from the alveolar crest (including the bone graft) were -1.7±0.5 mm in the SL group and -1.8±0.4 mm in the DL group, and the horizontal changes in the other areas were also similar in the DL and SL groups. The reductions in height were also comparable between groups.
CONCLUSIONS
Within the limitations of this study, single-layer and double-layer coverage with collagen membranes after ARP failed to show substantial differences in the preservation of horizontal or vertical dimensions or in clinical healing. Thus, both approaches seem to be suitable for open-healing ridge preservation procedures. Read More
3. Use of a Sugar-Crosslinked Collagen Membrane in Conjunction With a Dehydrated Amnion/Chorion Membrane for Guided Bone Regeneration Around Immediate Implants., Matthew J Fien , Israel Puterman , Juan Mesquida , Ferran Llansana Fitó , Guillermo Bauza , Compendium of continuing education in dentistry (Jamesburg, N.J. : 1995). Volume: 43, Issue: 5, 2022
Several bioabsorbable membranes have been proposed to exclude soft-tissue ingrowth and to stabilize the bone graft when guided bone regeneration (GBR) is performed. The properties of the various membranes differ slightly due to variances in composition and manufacturing processes affecting their handling and suitability for specific techniques. The aim of this article is to present a technique to perform GBR with the use of a sugar-crosslinked absorbable collagen membrane in conjunction with a dehydrated amnion/chorion membrane (dHACM). This technique can be used to perform GBR at the time of tooth extraction and for ridge augmentation of an edentulous site in preparation for future dental implant placement. The use of a collagen membrane in combination with a dHACM can facilitate stabilization of the bone graft and membrane by providing the benefits of a long-lasting bioabsorbable collagen membrane in addition to the unique benefits of an amnion/chorion membrane, which has been shown to provide growth factors to the surgical site that have potential to enhance regenerative outcomes. Read More4. Chorion and amnion/chorion membranes in oral and periodontal surgery: A systematic review., Sarah Gulameabasse , Florelle Gindraux , Sylvain Catros , Jean-Christophe Fricain , Mathilde Fenelon , Journal of biomedical materials research. Part B, Applied biomaterials. Volume: 109, Issue: 8, 2021
The aim of this study was to perform a systematic review on the clinical applications where chorion membrane (CM) and amnion/chorion membrane (ACM) were used for oral tissue regeneration procedures. Selection of articles was carried out by two evaluators in Pubmed and Scopus databases, and Outcomes (PICO) method was used to select the relevant articles. Clinical studies reporting the use of CM or ACM for oral soft and hard tissue regeneration were included. The research involved 21 studies conducted on 375 human patients. Seven clinical applications of CM and ACM in oral and periodontal surgery were identified: gingival recession treatment, intrabony and furcation defect treatment, alveolar ridge preservation, keratinized gum width augmentation around dental implants, maxillary sinus membrane repair, and large bone defect reconstruction. CM and ACM were compared to negative controls (conventional surgeries without membrane) or to the following materials: collagen membranes, dense polytetrafluoroethylene membranes, platelet-rich fibrin membranes, amnion membranes, and to a bone substitute. Several studies support the use of CM and ACM as an efficient alternative to current techniques for periodontal and oral soft tissue regeneration procedures. However, further studies are necessary to increase the level of evidence and especially to demonstrate their role for bone regeneration. Read More5. Evaluation of Regenerative Efficacy of Amnion and Chorion Membrane in Treatment of Mandibular Molar Furcation Defects: A Clinico-radiographic Study., Siddharth Mallapragda , Radhika Gupta , Stuti Gupta , Himani Sharma , Saransh Srivastava , Anusha Raj , The journal of contemporary dental practice. Volume: 25, Issue: 2, 2024
AIM
Amnion and chorion membranes possess unique inherited biological properties that enhance wound healing and may accelerate periodontal regeneration. The present study aims to evaluate and compare the efficacy of amnion and chorion membranes in the treatment of furcation defects.
MATERIALS AND METHODS
A total of 20 patients were selected and were randomly allocated to group I and group II with 10 subjects in each group. Amnion and chorion membranes are placental-derived membranes that accelerate regeneration by having natural growth factors with their antimicrobial and inflammation reduction properties. Group I was treated using bone grafting with decalcified freeze-dried bone allograft (DFDBA) and placement of amnion as a membrane for guided tissue regeneration (GTR) whereas group II was treated using bone grafting with DFDBA and placement of chorion as a membrane for GTR. The patients were followed for clinical and radiographic parameters and were evaluated between 3 and 6 months after surgery.
RESULT
In intragroup comparison, a significant difference was evident in both the groups for all the clinical and radiographic parameters within the groups. (, = 0.01) This means both amnion and chorion membranes showed statistically significant regenerative efficacy. In intergroup comparison, the results show that all the clinical parameters and radiographic parameters show no significant difference between the groups.
CONCLUSION
The amnion and chorion membranes had similar regenerative efficacy in combination with DFDBA in patients with buccal degree II furcation defects in mandibular molars.
CLINICAL SIGNIFICANCE
The amnion and chorion membranes have shown significant improvement in clinical and radiographic parameters when used for the treatment of buccal degree II furcation defects in mandibular molars. How to cite this article: Mallapragda S, Gupta R, Gupta S, et al. Evaluation of Regenerative Efficacy of Amnion and Chorion Membrane in Treatment of Mandibular Molar Furcation Defects: A Clinico-radiographic Study. J Contemp Dent Pract 2024;25(2):160-167. Read More
6. A Randomized Split-Mouth Clinical Trial on Effectiveness of Amnion-Chorion Membranes in Alveolar Ridge Preservation: A Clinical, Radiologic, and Morphometric Study., Muyeenul Hassan , Sivaraman Prakasam , Carol Bain , Ahmed Ghoneima , Sean Shih-Yao Liu , The International journal of oral & maxillofacial implants. Volume: 32, Issue: 6, 2017 Nov/Dec
PURPOSE
Recent case reports suggest that amnion-chorion membranes (ACM) and dense polytetrafluoroethylene membranes (dPTFE) can be left exposed during ridge preservation. The aim of this study was to compare the effectiveness of these membranes in ridge preservation, particularly when they are intentionally left exposed.
MATERIALS AND METHODS
A split-mouth, single-blind, randomized trial design was used to compare treatments with the two membranes in 22 nonmolar sites on the same arch. Ridge dimensions were recorded clinically and with cone beam computed tomography prior to and 3 months after ridge preservation. Postoperative discomfort was recorded with Visual Analog Scale (VAS) forms. Mixed‑model analysis of variance was used to test significance.
RESULTS
Clinical and radiographic ridge dimensions were not significantly different between the two treatments. ACM sites had significantly more osteoid and higher bone volume density but significantly less graft particles and bone surface density compared with dPTFE. Mineralized bone area and soft tissue area were not significantly different between the two treatments. ACM sites had significantly lower postoperative VAS scores compared with dPTFE.
CONCLUSION
Intentionally exposed ACM is equally effective in ridge preservation compared with dPTFE. Additionally, ACM use may aid in reducing postoperative VAS scores, and potentially result in better quality of bone available for implant placement, as evidenced by improved histomorphometric measures. Read More
7. Evaluation and Comparison of Human Chorionic Amniotic Membrane and Platelet-Rich Fibrin in Achieving Bone Formation and Soft Tissue Healing in Extraction Sockets Indicated for Rehabilitation with Implants: A Preliminary Study., Ratima Chopra , Kalyani Bhate , Nishtha Gadkari , Pradnya Kakodkar , Deepak Kulkarni , The International journal of oral & maxillofacial implants. Volume: 36, Issue: 2, 2021 Mar-Apr
PURPOSE
To evaluate and compare human chorionic amniotic membrane and platelet-rich fibrin on new bone formation and soft tissue healing in extraction sockets indicated for rehabilitation with dental implants.
MATERIALS AND METHODS
A prospective, triple blind clinical study was conducted. The inclusion criteria were as follows: patient with two extraction sites each in the same arch, intact buccal bone and soft tissue around the socket, and recommended rehabilitation with dental implants. Postextraction, the sockets were randomly placed with human chorionic amniotic membrane in one site and platelet-rich fibrin in the other site. After 3 months, a trephine drill was used to take a biopsy of the respective sites for soft and hard tissue samples. The outcome parameters that were assessed histologically were percentage of new bone formation and lymphocyte density.
RESULTS
After screening 80 patients, eight participants were recruited for the study. The mean percentage of new bone formation in the human chorionic amniotic membrane group was 45.71% ± 4.82%, and for the plasma-rich fibrin group, it was 41.39% ± 6.29%, showing no statistically significant difference (z = 0.99, P = .31). In the human chorionic amniotic membrane group, six out of eight sites had mild lymphocyte density, while the plasmarich fibrin group had equal numbers of mild and moderate lymphocyte density. No statistically significant difference between the groups (Fischer test value = 0.60, P = .25) was noted.
CONCLUSION
Within the limitations of the study, the results showed that there is no difference in the efficiency of human chorionic amniotic membrane compared with platelet-rich fibrin in achieving new bone formation and soft tissue healing in the extraction socket. Read More
8. Maxillary Sinus Membrane Repair With Amnion-Chorion Barriers: A Retrospective Case Series., Dan Holtzclaw , Journal of periodontology. Volume: 86, Issue: 8, 2015
BACKGROUND
Schneiderian membrane perforation is the most common complication of maxillary sinus augmentation procedures and has been associated with a variety of post-surgical problems. Multiple techniques to repair perforated Schneiderian membranes with materials such as connective tissue, buccal fat pads, and resorbable collagen membranes have been reported in the dental literature. Although these reparative options have proven successful, they are technique sensitive and time consuming. The aim of this case series is to present a simplified method of Schneiderian membrane perforation repair with amnion-chorion membranes and results obtained from nine cases using this technique.
METHODS
A consecutive retrospective record review was performed of all maxillary sinus augmentation cases performed during the past 5 years by the same board-certified private practice periodontist (DH).
RESULTS
Seventy-seven cases were identified, with a total of 104 sinus augmentations, in which nine perforations were noted. None of the perforation cases were aborted midprocedure, and all perforations were repaired with amnion-chorion membranes. All cases were augmented with a combination of allograft and xenograft particulate bone. After an average healing time of 4.9 months, dental implants were placed in the grafted sinuses.
CONCLUSIONS
This retrospective case series shows nine perforations during 104 lateral window maxillary sinus augmentation procedures. A total of 23 dental implants were placed in the augmented sinuses with perforated Schneiderian membranes, and one failure was noted according the Albrektsson success criteria. A total of 158 dental implants were placed in non-perforated augmented sinuses, with a total of three failures noted. Read More