This post reviews a case and provides a short interview with an expert on our Cytoflex Tefguard Membrane. Also see: Microporous PTFE Membranes for Vertical Augmentation
Case
MINIMALLY INVASIVE IMPLANT SITE GRAFTING TECHNIQUE Jenchun Chen DDS
This is a 38 year-old female who presented with a crown-root fracture of the mandibular first molar and a thin gingival biotype. An immediate implant placement following tooth extraction was planned. A flapless, minimally invasive extraction and implant placement combined with guided tissue regeneration was employed to minimize soft and hard tissue recession.
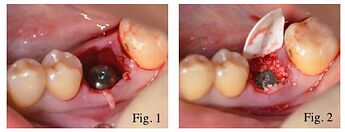
The tooth root was extracted with an intrasucular incision and a periosteal elevator. The extraction socket was curetted to remove all soft tissue remnants. After an implant was placed into the extraction site, the gap between the implant and the socket wall was filled with bone graft particles (Figures 1 & 2). A Tefguard® ePTFE membrane was trimmed to extend 3 mm beyond the socket walls and then tucked subperiosteally under the lingual flap, the buccal flap and underneath the interdental papilla using a curette.
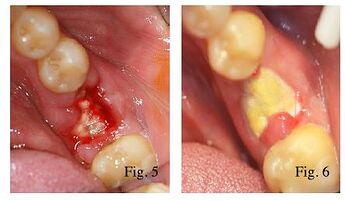
The membrane was allowed to rest passively over the socket (Figure 3), and was stabilized with a criss-cross absorbable PGA monofilament suture without primary closure (Figure 4). After one-week post operation, the graft site was uneventful, and the suture was removed (Figure 5). At three-week post-operation, the soft tissue overlying the exposed membrane demonstrated healing without signs of inflammation. An inadvertent fold in the membrane (introduced during membrane placement) was found at the distal buccal corner (Figure 6).
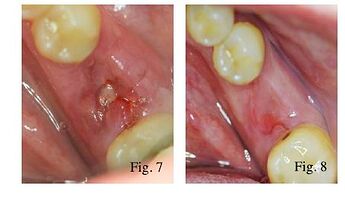
The decision was made to remove the membrane early to prevent potential complications as a result of the folding of the membrane. After applying topical anesthetic, the membrane was easily removed by grasping with a tissue forcep. A dense, vascular connective tissue matrix was found underlying the membrane in the extraction socket upon membrane removal. Figure 7 shows the site at one week after membrane removal.
Following membrane removal, keratinized gingiva began to form over the grafted socket. At six-week post-operation, the soft tissue was stable with preserved interproximal papillae and natural mucogingival architecture (Figure 8). This case demonstrates the use of a less invasive grafting technique using a micro porous ePTFE barrier.
Interview with an Expert
Below is an interview with Dr. David Kao, Periodontics and Dental Implants
Fullerton, CA about Cytoflex Tefguard
How long have you used non-resorbable Cytoflex® Tef-Guard® products?
What do you use the products mostly for?I have used the products since 2011. Mostly I used them for socket grafting with the non-primary closure technique.Do you notice any differences between smooth versus textured Cytoflex® Tef-Guard® products?
For the way I use Tef-Guard® in my office, I have not noticed little clinical differences in the smooth and textured. The handling property of the textured membrane is a bit improved over the smooth version. I find that the textured membrane is more durable. This does allow it to withstand the pressures tucking the membrane in below the gingiva. I also find that I can trim it better, but only marginally better. I will continue to use smooth only for its cost savings. Note: The Smooth version is no longer available, so this question is not so relevant anymore.In your experience, what is the best way to use the product? Do you under-fill the bone graft or fill to the crest level of the bone before applying the membrane? What suturing technique do you use over the membrane? What kind of sutures do you use to close the wound?
In my experience, the best way to use the product is to stabilize the membrane by extending about 3 mm between the bone and the labial and lingual flaps. If the interdental papillae were not elevated, then a suture would not be necessary. If a suture were necessary, I would utilize a mattress suture over the membrane (either cris-cross or parallel). I commonly use a resorbable suture, such as chromic gut. I have tried both under-filling and over-filling. With the over-fill technique, it is common to experience non-integrated bone graft at the crest. I am inclined to say that under-filling works well.I generally achieve good bone regeneration after 4-5 months of healing with just an allogenic bone graft (FDBA), Tef-Guard® membrane without primary closure in an intact tooth socket or a socket with minimal bone loss.
How long do you leave the membrane in place?
I try to leave the membrane in place for 4 weeks. After four weeks, you would get a moderately mature connective tissue with a few spicules of bone graft integrated in it. However, all cases end up with fully mature gingiva. After the removal of the membrane, the patient is advised to resume normal activity. No painkiller or dressings are needed.
What is the best way to remove the membrane? What instruments do you use?
I remove it by first lifting the membrane with a periodontal probe and extract it with cotton forceps.
Have you experienced any wound dehiscence while using this membrane? If so, what do you think caused the dehiscence? Any thoughts to prevent such complications?
I have not experienced wound dehiscence with the non-primary closure technique. In general, wound dehiscence is caused by injury (either during or after the procedure), poor blood supply, or thin tissue.Do you find Cytoflex® Tef-Guard® easy to use?
I do like the ease of use and would recommend Tef-Guard® products for socket grafting without primary closure.