This Week in Dental Implants, we want to highlight a new study that addresses the age-old question: Which sinus lift technique is preferable: Crestal (Indirect) or Lateral (Open/Direct)? Both surgical techniques are used to increase the height of bone in the posterior maxilla for dental implant placement, but they differ in their approach and execution.
The crestal sinus lift technique involves accessing the sinus through the crest of the alveolar ridge. This method is generally less invasive, as it utilizes a smaller incision and can often be performed simultaneously with implant placement. The procedure typically involves the use of osteotomes to elevate the sinus membrane and may involve bone grafting material to support the newly created space.
In contrast, the open or lateral sinus lift technique requires a larger incision on the side of the maxilla to create a window into the sinus cavity. This approach allows for direct access to the sinus membrane, which is then lifted, and bone graft material is placed beneath it. While this method is considered reliable and predictable, it may involve a higher risk of complications, such as perforation of the Schneiderian membrane.
So which procedure provides better clinical results? A new clinical trial, Implant Outcomes in Crestal Versus Open Sinus Elevation: A Randomized Clinical Trial, sheds light on that question. (Note: Since this was a clinical study, the entire study is described in detail on ClinicalTrials.gov)
The study concluded as follows:
The crestal sinus lifting technique using osteotomes, performed simultaneously with implant placement and allogenic bone grafting, shows only superior clinical outcomes of BI (bleeding index), radiographic outcomes of buccal bone changes, and patient-centered and reported outcomes of edema compared to the open sinus lifting technique. Therefore, the findings suggest that, while the crestal approach demonstrates certain advantages, both techniques can be considered for managing crestal bone heights ranging from four to seven millimeters, providing surgeons with two viable options for dealing with such reduced bone heights…The technique of choice where the maxillary sinus had pneumatized, especially in areas where the residual bone height ranges from four to seven millimeters, is debatable. Our study presents crestal sinus versus open sinus augmentation as a less invasive alternative that may provide similar results.1
Case Snippets
Direct Sinus Lift
Case photos provided by: Balaji SM. Direct v/s Indirect sinus lift in maxillary dental implants. Ann Maxillofac Surg. 2013 Jul;3(2):148-53.
Direct sinus lift with simultaneous implant placement with use of autogenous bone graft (a) In-fracturing and lifting of lateral window of right maxillary sinus, (b) Autogenous bone harvested from donor site being placed in newly created space, (c) Bone packed in the window, (d) Sinus floor augmented and implant placed
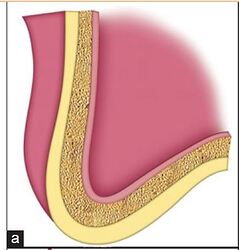
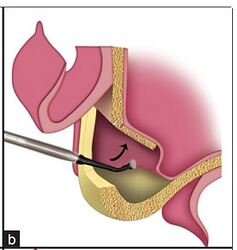
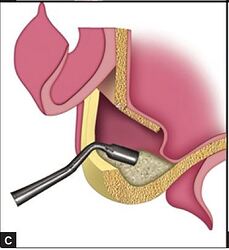
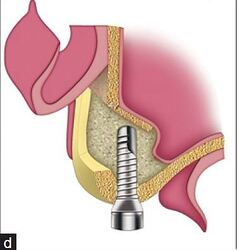
Line diagrams illustrating direct sinus lift with simultaneous implant placement, (a) Atrophic posterior maxilla with residual bone height between sinus floor and alveolar crest inadequate for placement of dental implant, (b) Lateral wall of sinus in-fractured and membrane is elevated, (c) Grafted bone is densely packed in space created after lifting the membrane, (d) Augmented maxillary sinus with implant placed
Indirect/Crestal Sinus Lift
Case photos provided by: Balaji SM. Direct v/s Indirect sinus lift in maxillary dental implants. Ann Maxillofac Surg. 2013 Jul;3(2):148-53.
Pre- and postoperative orthopantomograph (OPG) in a case treated with indirect sinus lift and bone graft for implant placement, (a) Insufficient residual bone, (b) After prosthetic rehabilitation following indirect sinus lift, bone grafting, and implant placement
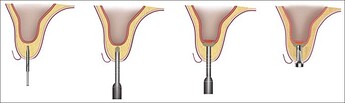
Sequential steps in indirect sinus augmentation technique; implant site prepared starting from small diameter to large diameter drills, sinus floor fractured, elevated, and bone graft placed in the resultant space and immediate implant placement
References
Implant Outcomes in Crestal Versus Open Sinus Elevation: A Randomized Clinical Trial., Hebatallah Mattar , Tamer A Nasr , Khaled M Keraa , Mohammed El Sholkamy , The International journal of oral & maxillofacial implants. Volume: 0, Issue: 0, 2025
PURPOSE
This study aimed to evaluate clinical, radiographic, patient-centered, and patient- reported outcomes of dental implants placed with maxillary sinus bone augmentation using two different sinus floor elevation techniques in reduced residual bone height of four to seven millimeters.
MATERIALS AND METHODS
Thirty implants were placed in conjunction with raising thirty maxillary sinuses in seventeen patients with residual bone heights of four to seven millimeters determined to be primarily due to sinus pneumatization rather than post-extraction resorption, as evidenced by the pre-operative CBCT analysis and comparison to neighboring alveolar bone level heights, with either crestal (indirect/osteotome) or open (direct/lateral window) sinus augmentation using allograft material. Patients were randomly assigned to the test group (crestal technique) or the control group (open technique). A 12-month follow-up assessed dental implant stability through Resonance Frequency Analysis (RFA) and monitored plaque, bleeding indices, and peri-implant probing depths. Changes in vertical, crestal, and buccal bone around the implants were examined after surgery, at six and at 12 months using low-dose Cone Beam Computed Tomography (CBCT) with a fusion module. Additionally, relative radiographic bone density was evaluated utilizing specialized software at six, nine and 12 months. Finally, the patient-centered outcome of edema was objectively measured as well as subjectively reported by the patient.
RESULTS
After 12 months of follow-up, no significant differences were observed between the groups regarding radiographic parameters. There were no statistically significant differences in ISQ scores or implant success/failure rates (p>0.05). Clinically, the test (crestal) group exhibited a lower bleeding index (BI) (p=0.027) and more favorable edema outcome scores, measured by both patient-centered and patient-reported methods, compared to the control group (p=0.016 and 0.003, respectively).
CONCLUSIONS
The crestal sinus lifting technique using osteotomes, performed simultaneously with implant placement and allogenic bone grafting, shows only superior clinical outcomes of BI, radiographic outcomes of buccal bone changes, and patient-centered and reported outcomes of edema compared to the open sinus lifting technique. Therefore, the findings suggest that, while the crestal approach demonstrates certain advantages, both techniques can be considered for managing crestal bone heights ranging from four to seven millimeters, providing surgeons with two viable options for dealing with such reduced bone heights. This clinical trial was registered on ClinicalTrials.gov (ID: NCT06265467).
CLINICAL RELEVANCE
The technique of choice where the maxillary sinus had pneumatized, especially in areas where the residual bone height ranges from four to seven millimeters, is debatable. Our study presents crestal sinus versus open sinus augmentation as a less invasive alternative that may provide similar results. Read More
1-stage versus 2-stage lateral sinus lift procedures: 1-year post-loading results of a multicentre randomised controlled trial., Pietro Felice , Roberto Pistilli , Maurizio Piattelli , Elisa Soardi , Carlo Barausse , Marco Esposito , European journal of oral implantology. Volume: 7, Issue: 1, 2014 Spring
PURPOSE
To compare the efficacy of 1-stage versus 2-stage lateral maxillary sinus lift procedures.
MATERIALS AND METHODS
Sixty partially edentulous patients requiring 1 to 3 implants and having 1 to 3 mm of residual bone height and at least 5 mm bone width below the maxillary sinus, as measured on CT scans were selected. They were randomised according to a parallel group study design into two equal arms to receive either a 1-stage lateral window sinus lift with simultaneous implant placement or a 2-stage procedure with implant placement delayed by 4 months, using a bone substitute in three different centres. Implants were submerged for 4 months, loaded with reinforced provisional prostheses, which were replaced, after 4 months, by definitive prostheses. Outcome measures, assessed by masked assessors, were: augmentation procedure failures; prosthesis failures and implant failures; complications; and marginal peri-implant bone level changes. Patients were followed up to 1 year after loading. Only data of implants placed in 1 to 3 mm of bone height were reported.
RESULTS
Two patients dropped out from the 1-stage group and none from the 2-stage group. No sinus lift procedure failed in the 1-stage group but one failed in the 2-stage group, the difference being not statistically significant (P = 1.00). Two prostheses failed or could not be placed in the planned time in the 1-stage group and one in the 2-stage group, the difference being not statistically significant (P = 0.51). Three implants failed in three patients of the 1-stage group, versus one implant in the 2-stage group, the difference being not statistically significant (P = 0.28). Two complications occurred in the 1-stage group and one in the 2-stage group, the difference being not statistically significant (P = 0.61). One year after loading, 1-stage treated patients lost an average of -1.01 mm (SD: 0.56) of peri-implant bone and 2-stage sites about -0.93 mm (SD: 0.40). There were no statistically significant differences in bone level change between groups 1 year after loading (-0.08 mm 95%CI: -0.33 to 0.18 P = 0.56).
CONCLUSION
No statistically significant differences were observed between implants placed according to 1- or 2-stage sinus lift procedures. However this study may suggest that in patients having residual bone height between 1 to 3 mm below the maxillary sinus, there might be a slightly higher risk for implant failures when performing a 1-stage lateral sinus lift procedure. Read More
Maxillary Sinus Lift Procedures: An Overview of Current Techniques, Presurgical Evaluation, and Complications., Abdulrahman M Alshamrani , Mazen Mubarki , Abdulelah S Alsager , Hussam K Alsharif , Saud A AlHumaidan , Ahmad Al-Omar , Cureus. Volume: 15, Issue: 11, 2023
A maxillary sinus lift procedure is indicated if a dental implant needs to be placed in the posterior maxilla with limited bone available to accommodate a dental implant. Both open and closed sinus lifting procedures are reliable approaches for increasing the bone volume needed to support proper implant positioning. However, these methods can lead to several complications. In addition to the general complications commonly linked to oral surgery, such as swelling or hematoma, the primary complication in open sinus lifting is typically the perforation of the Schneiderian membrane during osteotomy. Detailed and extensive presurgical evaluation is crucial to minimize such complications. The objective of this study was to delineate contemporary trends in sinus lift surgery, with a specific emphasis on different techniques of sinus lift procedure, anatomical and surgical factors, presurgical evaluation, bone grafting, and the practical implications of these factors in implant dentistry cases involving a deficient posterior maxilla. In conclusion, while both osteotome and lateral window techniques can assist clinicians in addressing the complexities of implant placement in a deficient posterior maxilla, bone height before implantation remains a critical factor in determining the success and longevity of implants. Read MoreDirect v/s Indirect sinus lift in maxillary dental implants., S M Balaji , Annals of maxillofacial surgery. Volume: 3, Issue: 2, 2013
INTRODUCTION
Lack of sufficient bone height along maxillary sinus poses significant difficulty for placement of implants in edentulous maxillary jaw. Minimally invasive sinus augmentation is an effective solution for this problem. The manuscript intends to present long period results of such augmentation using direct (DSAT) and indirect (ISAT) minimally invasive sinus augmentation technique (SAT) from a single center.
MATERIALS AND METHODS
Records of patients who required minimally invasive sinus augmentation to increase residual bone height for implant placement fulfilling predetermined exclusion and inclusion criteria. Only patients with follow-up records for at least a year were considered. Both DSAT and ISAT were employed for sinus augmentation. The age, gender, period of edentulousness, alveolus thickness at crestal level during the pre- and postoperative assessment, implant length, and diameter of implants were collected from case histories. Descriptive statistics, Chi-square, paired test, and one way analysis of variance (ANOVA) was used appropriately. P ≤ 0.05 was considered as significant.
RESULTS
There were 197 implants placed and mean age of the group was 40.2 ± 10.7 years. There was a slight male predilection (54.3%). The gain in bone height as expressed in percentage after a year was 134.6%. On comparing the length of residual alveolar bone (RAB) at start and end of study, ISAT had a mean preoperative height of 7.88 mm while postoperative height was 13.22 mm. For DSAT, the mean height at start of treatment was 3.94 mm while at the end it was 10.13 mm. The mean increase in height was 6.19 mm. For both cases, P was 0.000.
DISCUSSION
Age, gender, and period of edentulism did not influence the outcome. The alveolar width appears to differ and influence the outcome. When alveolar width increases, wider diameter implants can be placed by compromising height. Thus it is a clinical acumen that would be extremely helpful to gauge the outcome of the condition. Read More