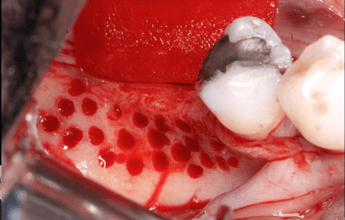
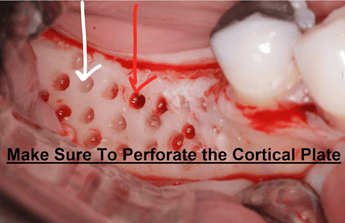
Cortical bone perforation (sometimes also called intramarrow penetration) refers to the intentional creation of small holes in the cortical bone. It aims to enhance angiogenesis and osteogenesis during guided bone regeneration procedures. By mechanically perforating the cortical surface of the bone, it is believed that the increased surface area and access to the medullary cavity can facilitate better blood supply and nutrient flow to the grafted area. This can potentially lead to improved healing and integration of the graft with the host bone.
Discussion
While the practice of perforating cortical bone before bone grafting is an accepted component of the GBR procedure, is it really necessary? The reality is that the research on cortical bone perforation is not definitive. An initial review of the technique by Tarnow in 2009 concluded that: “There is conflicting information and not enough clinical trials to make a definitive determination as to the merits of bone decortication prior to GBR procedures.” 1 Another study concluded that the area of decortication is important with different results for the maxilla vs mandible with a further study from Tarnow in 2017 with osseous defects in the mandible stating that: “Cortical bone perforation significantly increase number of new vessels (angiogenesis) of the regenerated bone.” 2,3 However, more recent studies have been inconclusive with a larger study of 26 patients with block grafts demonstrating that, “cortical perforations of the recipient site in the maxilla did not improve angiogenesis nor bone formation within the block graft.” 4 Given all the conflicting information, we were pleased to find a recent systematic review with meta-analysis that was published in January 2025 after comparing 653 articles on the topic. The conclusion was interesting in that the authors found that while the clinical evidence for the benefits of cortical perforation was poor, there were no negative effects reported from the procedure. As such since increasing blood supply to the site may help healing, intramarrow perforations should be considered in some procedures. 5
Case Presentation: Understanding Cortical Perforations
This is a great case presentation from Dr. Daniel Gober on Cortical perforations. He explains the rationale behind the procedure, discusses when he thinks they might be very important (i.e. the mandible) to ensure adequate blood supply, why sometimes the technique is not indicated.
References
1. The role of bone decortication in enhancing the results of guided bone regeneration: a literature review., G Greenstein , B Greenstein , J Cavallaro , D Tarnow , Journal of periodontology. Volume: 80, Issue: 2, 2009
|:: BACKGROUND ::| |::: Bone decortication is often performed as part of a guided bone regeneration (GBR) procedure. The biologic rationale for decortication of bone is to allow progenitor cells easy access to a GBR-treated site and to facilitate prompt angiogenesis. It also may enhance the physical connection between a bone graft and a recipient site. However, the concept of decortication prior to a GBR procedure is controversial because there are no human clinical trials to support its effectiveness, and there are opposing points of view derived from animal studies regarding its usefulness. :::| |:: METHODS ::| |::: The literature was assessed to determine whether there are enough data to validate the rationale for using decortication of bone as an integral part of GBR procedures. Eight searches were performed seeking controlled clinical trials that addressed the ability of decortication to enhance GBR. :::| |:: RESULTS ::| |::: Three controlled animal clinical trials were found that supported the use of decortication prior to performing GBR. Two controlled animal clinical trials were located that indicated decortication did not improve GBR procedures. No human controlled clinical trial was identified that addressed the ability of decortication to alter GBR procedures. The literature addressing the capacity of decortication to affect onlay grafting or wound healing also provided mixed results. :::| |:: CONCLUSION ::| |::: There is conflicting information and not enough clinical trials to make a definitive determination as to the merits of bone decortication prior to GBR procedures. :::|
Read More2. The role of cortical perforations in bone regeneration: a systematic review., J Alvira-González , L De Stavola , International journal of oral and maxillofacial surgery. Volume: 49, Issue: 7, 2020
The aim of this review was to determine the effect of cortical perforations in bone regeneration considering the surgical technique. An electronic search in the PubMed (MEDLINE) and ScienceDirect databases and a hand search of the literature was conducted covering the period July 2008 to December 2018. Studies that specified the creation of perforations in the recipient area as a study variable associated with the regenerative technique were included. The quality of the randomized clinical trials included in this systematic review was also assessed. A total of 16 articles met both inclusion criteria and were eligible for analysis. Studies were grouped into three blocks according to the associated surgical technique. All studies were performed in an experimental model except for one. Qualitative assessment of the studies showed a moderate to high risk of bias of the overall studies. The evidence for creating perforations in guided bone regeneration and also in combination with autologous bone blocks in order to increase bone formation is limited according to the publications analysed. Although the number and size of perforations do not appear to interfere with the result, their effect in the upper maxilla and in the mandible should be evaluated separately due to the structural anatomical differences.
Read More3. The influence of cortical bone perforation on guided bone regeneration in humans., S A Danesh-Sani , D Tarnow , J K Yip , R Mojaver , International journal of oral and maxillofacial surgery. Volume: 46, Issue: 2, 2017
The purpose of this study was to evaluate the effect of cortical bone perforation on angiogenesis and osteogenesis of the augmented ridge in guided bone regeneration. Eighteen patients who had osseous defects in the mandible were selected. In the test group (n=9), alveolar cortical bone in the area of regeneration was perforated. No decortication was performed in the control group (n=9). Subsequently, defects were augmented by guided bone regeneration using resorbable membrane and bovine bone. After a healing period of 7 months, trephine cores were harvested for histological and histomorphometric analysis of the grafted areas. Histomorphometry demonstrated that the amount of newly formed bone in the test group (27.8%) was greater than that in the control group (25.3%), but the difference was not statistically significant (P=0.13). However, the mean number of microvessels in the test group was significantly higher than that in the control group (P=0.01). This study found that cortical bone perforation favourably affects the amount of new bone formation in the grafted sites after 7 months of healing. Cortical bone perforation significantly increase number of new vessels (angiogenesis) of the regenerated bone. Further randomized clinical trials are required to confirm these results.
Read More4. The role of cortical perforations in allogeneic block grafting for lateral augmentation in maxilla: A randomized clinical trial., Francisco G F Tresguerres , Isabel F Tresguerres , Oscar Iglesias , Isabel Leco , Faleh Tamimi , Jesús Torres , Clinical implant dentistry and related research. Volume: 23, Issue: 4, 2021
|:: BACKGROUND ::| |::: The need of decortication on the recipient site remains unclear for bone regeneration. To our knowledge, there are no human clinical trials that studied the influence of decortication on cancellous allogeneic block grafting. :::| |:: PURPOSE ::| |::: The aim of the present study is to evaluate the influence of perforating the cortex of the recipient site on cancellous allogeneic block graft integration and revascularization in the maxilla. :::| |:: MATERIAL AND METHODS ::| |::: Twenty-six patients referred for lateral bone augmentation were included in this clinical trial. Patients received freeze-dried bone allograft cancellous blocks obtained from the iliac crest; cortical perforations of the recipient bed were performed in the test group while in the control group it was left intact. After a 4-month healing period another surgery was performed to place dental implants, and a bone biopsy was collected using a trephine. All samples underwent micro-CT scans, and were processed for histomorphometric and immunohistochemical analysis. Implant survival comparisons were made using a repeated measures analysis of variance (ANOVA) while all other variables were compared using the analysis of covariance (ANCOVA). :::| |:: RESULTS ::| |::: One hundred and nineteen implants were placed into 110 augmented sites. One hundred percent implant survival rate was reported during 24 months follow-up period. No differences were reported in bleeding on probing at 1 (5.6 vs 9%) and 2 years (13.2 vs 12.1%), probing pocket depth at 1 (3.4 ± 0.95 vs 3.6 ± 1.12 mm) and 2 years (3.8 ± 1.02 vs 4.1 ± 1.46 mm), and marginal bone loss at 1 (0.2 ± 0.52 vs 0.3 ± 0.57 mm) and 2 years (0.6 ± 0.91 vs 0.5 ± 0.87 mm). No statistically significant differences were found in the micro-CT and histomorphometric analysis in terms of newly formed bone (25.7 ± 11.2% vs 22.3 ± 9.7%), soft tissue (33.0 ± 14.7% vs 36.5 ± 15.7%), remnant allograft (39.3 ± 20.4% vs 41.2 ± 22.7%), and bone mineralization (57.2 ± 10.6% vs 53.8 ± 8.7%). Perforating the cortex of the recipient site had no significant effect on angiogenesis as shown by immunohistochemical analysis of CD34 positive blood vessels (39.21 ± 10.53/mm, vs 34.16 ± 12.67/mm, ). :::| |:: CONCLUSION ::| |::: Cancellous allogeneic bone block grafts are a clinically acceptable alternative for horizontal bone augmentation. Cortical perforations of the recipient site in the maxilla did not improve angiogenesis nor bone formation within the block graft. :::|
Read More5. The clinical effect of bone perforations in periodontal regeneration and alveolar socket preservation: a systematic review with meta-analysisPaolo Pesce 1, Luigi Canullo 1, Tiziano Testori 2,3,4,5, Alessandro Mastroianni 6, Massimo Del Fabbro, Clin Oral Investig. 2025 Jan 16;29(1):64. doi: 10.1007/s00784-025-06152-4.
Cortical perforations showed no consistent benefits for promoting bone regeneration in alveolar preservation procedures and periodontal surgery compared to controls without perforation. Very few of the parameters investigated resulted in clinically relevant benefits but the evidence level remains poor. Anyway, no negative effects of such procedure, nor peri- and postsurgical complications, have been reported. As increasing bleeding at the healing sites may increase the availability of oxygen and nutrients, as well as of blood cells and platelet factors essential for promoting the healing process, intramarrow perforations might be considered in the procedures for the reconstruction of bone defects. Further comparative studies, with larger sample size, consisting of both animal and clinical prospective research, is needed to better establish the effects of decortication on the tissues and cells involved in the healing process, especially in guided bone regeneration procedures.
Read More