This Week in Dental Implants, we want to highlight a study from the Brånemark Clinic in Gothenburg, Sweden, that followed up on implant treatments from 1982-1985. The study caught our attention because it seems to be the longest follow up done on single dental implants.
Case Photo
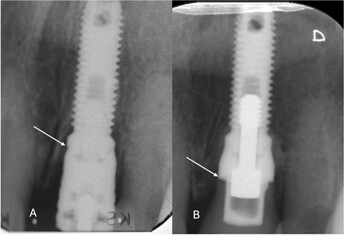
Radiographs collected at baseline with an acrylic crown (A) in 1984 and at the 40‐year follow‐up (B) with a cemented ceramic crown placed on a Nobel Brånemark CeraOne abutment. The arrows indicate the marginal bone levels (MBL) at baseline (A) and at the follow‐up visit (B), and show significant bone gain during the follow‐up period. Source: Outcome of Single Dental Implants Over 38-40 Years: A Long-Term Follow-Up Study., Sargon Barkarmo , Jan Kowar , Clinical implant dentistry and related research. Volume: 27, Issue: 1, 2025
Discussion
Millions of patients worldwide have received single implants. As many of the patients who receive these implants are young at the time of treatment, gathering long-term evidence supporting single dental implant treatment is crucial. While there are several studies with follow-up for 5, 10 or 15-years, there aren’t many studies for longer periods. The Branemark study followed up treatments for 16 patients that received single-tooth implants from 1982-1985. Out of the 16 patients, only 13 patients were available for follow-up. Despite the limited patient pool, we still think the study is illuminating.
The summary of the results were as follows:
The cumulative survival rates were 95.6% for the implants and 60.9% for the implant-supported crowns after 38-40 years in function. The marginal bone level changes were 0.9 ± 1.0 mm (range, -0.5─3.0 mm) over the follow-up period. The frequency of biological complications was low; although mucositis was common, no cases of peri-implantitis were observed. The mean plaque index was 16.9% ± 11.6% (range, 1%─34%) and the mean probing depth around the implants was 3.8 ± 2.2 mm (range, 0.0─7.0 mm). Few technical complications were observed, although many of the original implant-supported crowns had been replaced for esthetic reasons.
What is evident from the results is that single-tooth implants have a very favorable long-term survival rate at the implant level, but the the restorative treatment doesn’t have the same prognosis, and crown replacement may eventually be necessary. In addition, what struck us as especially noteworthy about the study, is the data surrounding the bone levels. Overall, the marginal bone loss showed only very small changes over time, and there was even bone gain in many of the implants!
Was 2-Stage Surgery a Factor?
Despite the excellent results, the authors of the study are correct in pointing out that the high survival rate may be due to the fact that the implants were placed with the 2-Stage surgical method, with average healing time between the two surgeries at 7 months. Can similar long-term results be expected nowadays when shorter treatment times are becoming more accepted and prevalent? Only time will tell.
References
Outcome of Single Dental Implants Over 38-40 Years: A Long-Term Follow-Up Study., Sargon Barkarmo , Jan Kowar , Clinical implant dentistry and related research. Volume: 27, Issue: 1, 2025
|:: INTRODUCTION ::| |::: This is a comprehensive, long-term follow-up study of single-implant treatments. At the Brånemark Clinic in Gothenburg, Sweden, during the period of 1982-1985, 16 patients received single-tooth implants. :::| |:: OBJECTIVE ::| |::: This study evaluates the survival rate of the implants after nearly four decades, focusing on the biological and technical complications. :::| |:: METHODS ::| |::: Of the original 16 patients with a total of 23 implants, 13 patients with 18 implants were available for the follow-up and were included in the study. Clinical and radiographic examinations were performed on these patients. :::| |:: RESULTS ::| |::: The cumulative survival rates were 95.6% for the implants and 60.9% for the implant-supported crowns after 38-40 years in function. The marginal bone level changes were 0.9 ± 1.0 mm (range, -0.5─3.0 mm) over the follow-up period. The frequency of biological complications was low; although mucositis was common, no cases of peri-implantitis were observed. The mean plaque index was 16.9% ± 11.6% (range, 1%─34%) and the mean probing depth around the implants was 3.8 ± 2.2 mm (range, 0.0─7.0 mm). Few technical complications were observed, although many of the original implant-supported crowns had been replaced for esthetic reasons. :::| |:: CONCLUSION ::| |::: The findings emphasize the importance of long-term follow-up in implant dentistry, particularly for younger patients, to improve understanding of potential complications and the longevity of treatment outcomes. Overall, single-tooth implants have a favorable long-term prognosis, though crown replacement may eventually be necessary. :::|
Read MoreReasons for failures of oral implants., B R Chrcanovic , T Albrektsson , A Wennerberg , Journal of oral rehabilitation. Volume: 41, Issue: 6, 2014
This study reviews the literature regarding the factors contributing to failures of dental implants. An electronic search was undertaken including papers from 2004 onwards. The titles and abstracts from these results were read to identify studies within the selection criteria. All reference lists of the selected studies were then hand-searched, this time without time restrictions. A narrative review discussed some findings from the first two parts where separate data from non-comparative studies may have indicated conclusions different from those possible to draw in the systematic analysis. It may be suggested that the following situations are correlated to increase the implant failure rate: a low insertion torque of implants that are planned to be immediately or early loaded, inexperienced surgeons inserting the implants, implant insertion in the maxilla, implant insertion in the posterior region of the jaws, implants in heavy smokers, implant insertion in bone qualities type III and IV, implant insertion in places with small bone volumes, use of shorter length implants, greater number of implants placed per patient, lack of initial implant stability, use of cylindrical (non-threaded) implants and prosthetic rehabilitation with implant-supported overdentures. Moreover, it may be suggested that the following situations may be correlated with an increase in the implant failure rate: use of the non-submerged technique, immediate loading, implant insertion in fresh extraction sockets, smaller diameter implants. Some recently published studies suggest that modern, moderately rough implants may present with similar results irrespective if placed in maxillas, in smoking patients or using only short implants.
Read MoreA systematic review of survival of single implants as presented in longitudinal studies with a follow-up of at least 10 years., Lars Hjalmarsson , Maryam Gheisarifar , Torsten Jemt , European journal of oral implantology. Volume: 9 Suppl 1, Issue: , 2016
|:: BACKGROUND ::| |::: Placement of single implants is one of the most common applications for implant treatment. Millions of patients have been treated worldwide with osseointegrated implants and many of these patients are treated at a young age with a long expected remaining lifetime. Therefore longterm evidence for such treatment is important. :::| |:: AIM ::| |::: To report patient treatment, implant and implant-supported single crown survival over at least a 10-year period of follow-up. :::| |:: MATERIAL AND METHODS ::| |::: After reviewing long-term publications, included by Jung et al (2012), a complementary PubMed search was performed using the same search strategy for the period September 2011 to November 2014. Data on implant and single implant crown treatment survival were compiled from included studies. :::| |:: RESULTS ::| |::: Four new publications were identified from the 731 new titles. They were added to an earlier list of five manuscripts by Jung et al (2012) , which were already included. Accordingly, nine publications formed the database of available long-term evaluations. The database consisted of 421 patients altogether, provided with 527 implants and 522 single crowns. From the 367 patients that were followed-up for at least 10 years (87%), altogether 502 implants were still in function at the completion of the studies (95.3%), supporting 432 original and 33 remade single implant crowns. Based on patient level and implant level data, implant survival reached 93.8% and 95.0%, respectively. The corresponding survival rate for original crown restorations was 89.5%. :::| |:: CONCLUSIONS ::| |::: Single implant treatment is a predicable treatment over a 10-year period of time, with no indication of obvious changes in implant failure rate between 5 and 10 years. However, replacement of new single crowns must be considered during the follow-up as part of regular maintenance. Compared to the number of treated patients worldwide, the available numbers with a follow-up of 10 years was low. :::|
Read MoreLong-term follow-up of turned single implants placed in periodontally healthy patients after 16-22 years: radiographic and peri-implant outcome., M Dierens , S Vandeweghe , J Kisch , K Nilner , H De Bruyn , Clinical oral implants research. Volume: 23, Issue: 2, 2012
|:: OBJECTIVES ::| |::: Retrospectively evaluate the survival, radiographic and peri-implant outcome of single turned Brånemark™ implants after at least 16 years. :::| |:: MATERIALS AND METHODS ::| |::: From 134 patients (C-group), 101 could be contacted concerning implant survival and 50 (59 remaining implants) were clinically examined (I-group). Marginal bone level was radiographically measured from the implant-abutment junction at baseline (=within 6 months after abutment connection) and 1-4, 5-8 and 16-22 years post-operatively. Probing depth, gingival and plaque index were measured. Marginal bone-level changes were analyzed using Friedman's and Wilcoxon's signed ranks tests. Spearman's correlations between radiographic and clinical parameters were calculated. :::| |:: RESULTS ::| |::: In the C-group, 13 out of 166 implants in 11 out of 134 patients failed (CSR=91.5%). In the I-group (28 males-22 females; mean age 23.9 years at baseline; range 14-57), the mean follow-up was 18.4 years (range 16-22). The mean bone level was 1.7±0.88 mm (range -0.8 to 5) after 16-22 years. Changes in the mean marginal bone level were statistically significant between baseline and the second measuring interval (1-4 years). Thereafter, no significant differences could be demonstrated. The mean interproximal probing depth, gingival and plaque indices were 3.9±1.27 mm, 1.2±0.81 and 0.2±0.48, respectively. Probing depth was moderately correlated with gingival inflammation (r=0.6; P<0.001) but not with bone level (P>0.05). 81.4% of the implants had a bone level ≤2nd thread and 91.5% had a probing depth ≤5 mm. 76.3% had both bone level ≤2nd thread and probing depth ≤5 mm. :::| |:: CONCLUSIONS AND CLINICAL IMPLICATIONS ::| |::: The single turned Brånemark™ implant is a predictable solution with high clinical survival and success rates. In general, a steady-state bone level can be expected over decades, with minimal signs of peri-implant disease. A minority (5%), however, presents with progressive bone loss. :::|
Read More